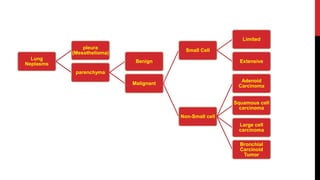
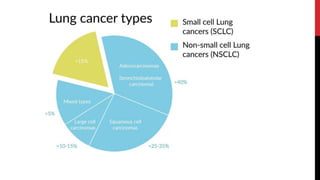
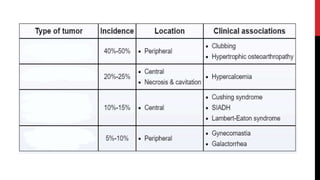
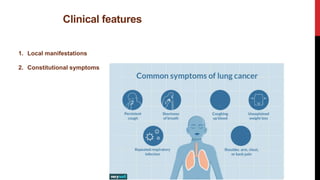
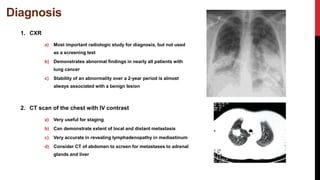
Lung cancer is the leading cause of cancer death worldwide, with smoking being responsible for about 90% of cases. There are two main types: primary lung cancer originating in the lungs and secondary lung cancer that has spread from other areas. Risk factors include smoking as well as exposure to radon, asbestos, and air pollution. Symptoms vary depending on whether the cancer is localized or has metastasized to other organs, with common sites of metastasis being the brain, liver, adrenal glands, and bones. Diagnosis involves imaging tests like CT and PET scans as well as biopsies of suspicious areas. Treatment depends on cancer type and stage but may include surgery, radiation, chemotherapy, and immunotherapy.