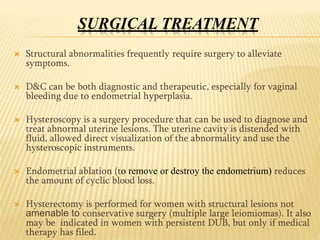
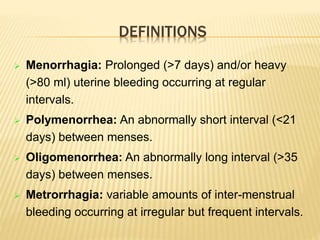
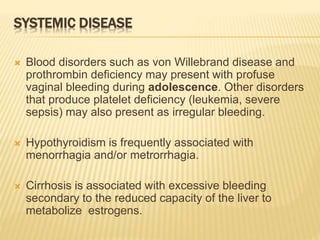
The document discusses abnormal vaginal bleeding and its definitions, including menorrhagia, polymenorrhea, and metrorrhagia, and outlines the causes, which range from dysfunctional uterine bleeding to systemic diseases. It emphasizes the importance of thorough diagnosis through patient history, physical examination, and various medical tests to rule out organic conditions. Treatment methods include medical options like hormonal therapies and non-steroidal anti-inflammatory drugs, as well as surgical interventions for structural abnormalities.










![DIAGNOSIS
Measurement of serum hemoglobin concentration,
iron levels, and ferritin levels is an objective measure
of the quantity and duration of menstrual blood loss.
Additional laboratory tests (TSH, coagulation profile)
may be indicated.
To determine whether bleeding is anovulatory or
ovulatory high progesterone levels during the luteal
phase suggests that ovulation has occurred.
Liver function tests if a liver disorder is suspected
endometrial biopsy or hysteroscopy.
A cervical cancer screening test (eg, Papanicolaou
[Pap] test, HPV test) if results are out-of-date
Testing for Neisseria gonorrhea and Chlamydia sp if
pelvic inflammatory disease or cervicitis is suspected](https://image.slidesharecdn.com/abnormalvaginalbleeding-161026223310/85/Abnormal-vaginal-bleeding-13-320.jpg)