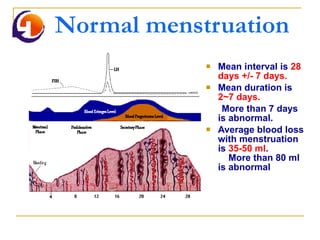
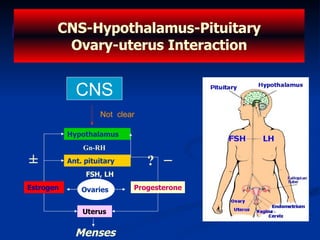
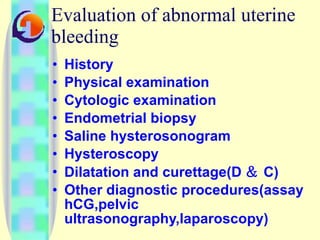
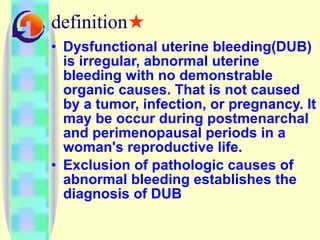
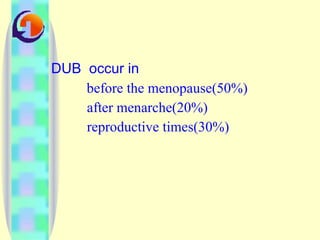
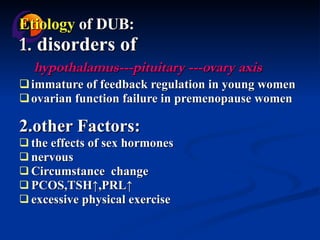
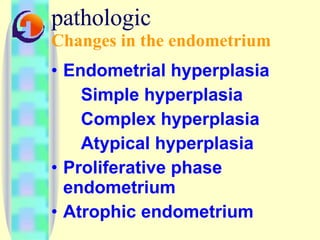
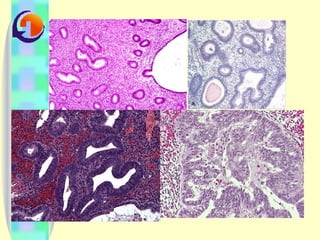
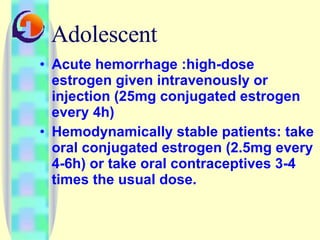
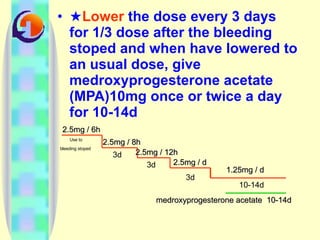
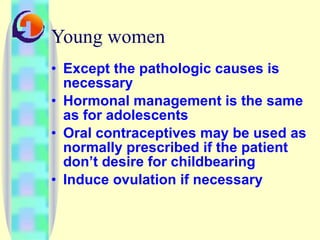
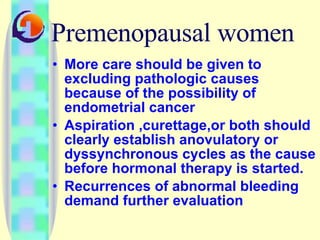
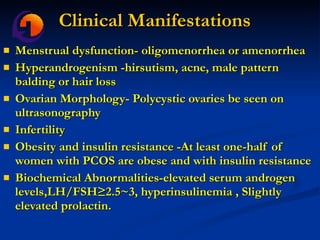
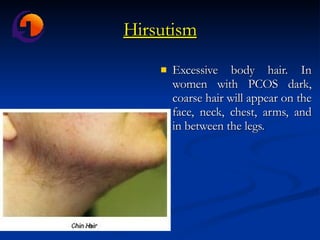
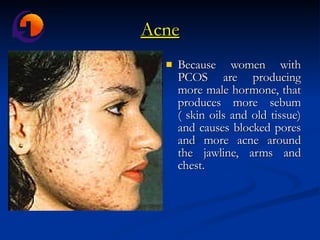
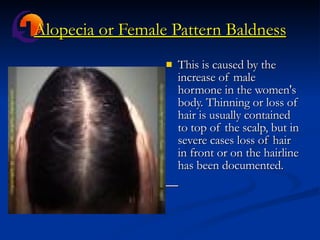
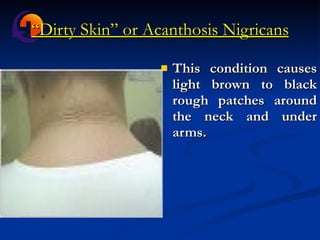
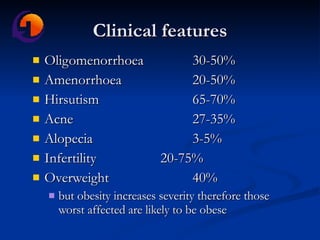
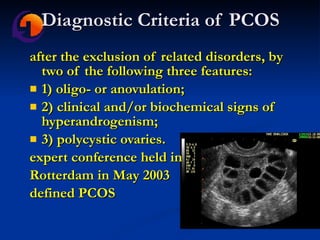
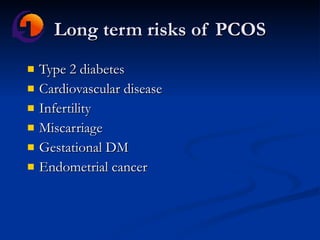
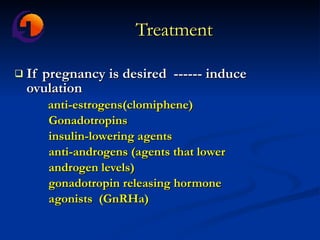
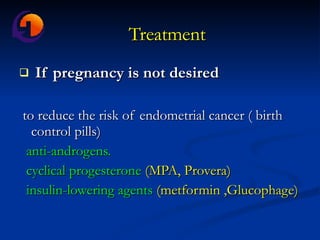
The document discusses normal and abnormal menstruation, including normal menstrual cycles, dysfunctional uterine bleeding, polycystic ovarian syndrome, and their causes, symptoms, diagnosis and treatment. It provides details on conditions like menorrhagia, metrorrhagia, oligomenorrhea and their definitions. PCOS is described as a syndrome characterized by menstrual irregularity, hyperandrogenism and polycystic ovaries. Long term risks of PCOS include diabetes, heart disease and infertility.