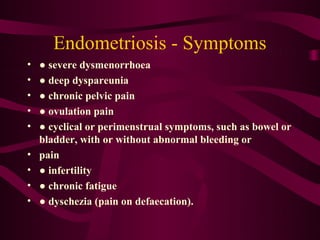
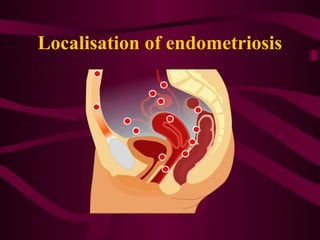
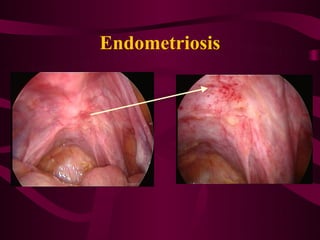
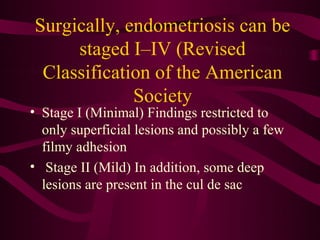
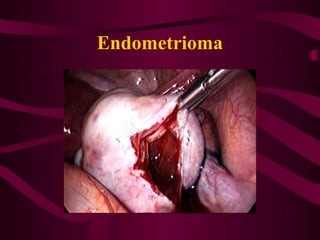
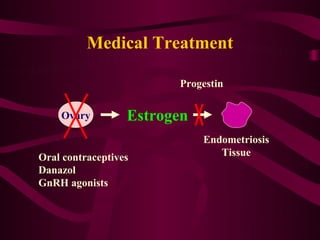
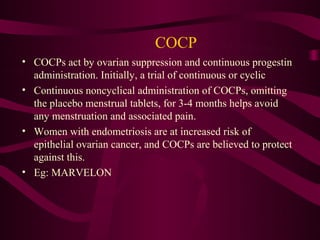
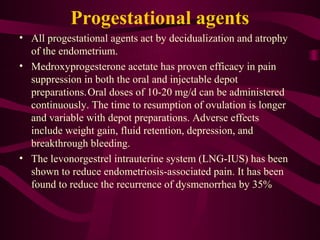
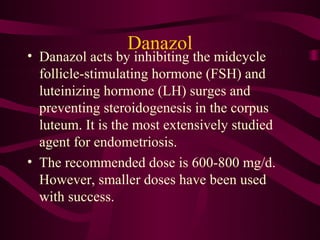
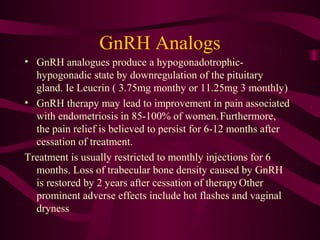
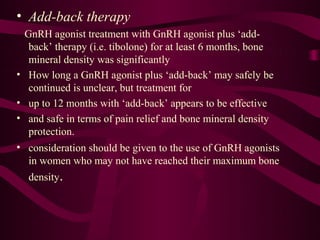
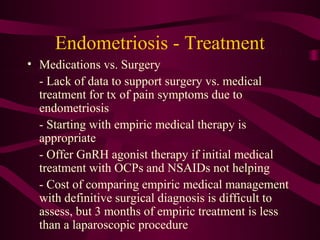
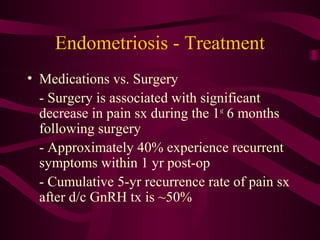
Endometriosis is defined as the presence of endometrial-like tissue outside the uterus, which induces chronic inflammation and can cause severe pelvic pain and infertility. A definitive diagnosis requires laparoscopic visualization and biopsy of lesions. Treatment involves hormonal medications like oral contraceptives or GnRH analogues to suppress ovarian function, or surgery to remove lesions and adhesions.