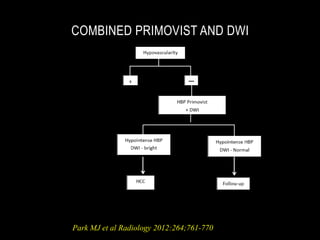
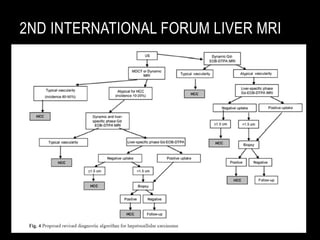
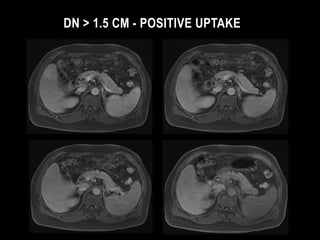
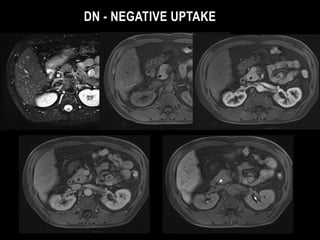
This document discusses the current approach for diagnostic imaging of small hepatocellular carcinoma (HCC) in patients with liver cirrhosis using gadoxetic acid (Primovist) enhanced magnetic resonance imaging (MRI) and diffusion weighted imaging (DWI). It summarizes that the combined use of Primovist MRI and DWI provides high diagnostic accuracy and sensitivity, particularly for detecting HCC lesions smaller than 2cm. This approach can image the step-wise progression of hepatocarcinogenesis by assessing vascularity, hepatocyte function, and cell density. The summary highlights that while Primovist MRI alone has high sensitivity, it has compromised specificity, but combining it with DWI increases specificity by differentiating HCC from