This document provides information on assessing and managing critically ill patients using the ABCDE approach. It discusses:
- Common early signs of critical illness including hypoxia and hypotension.
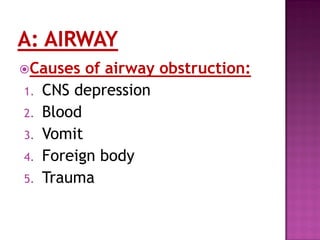
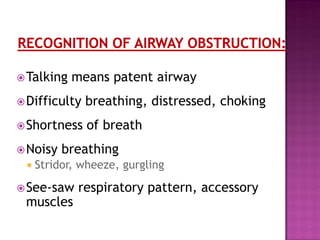
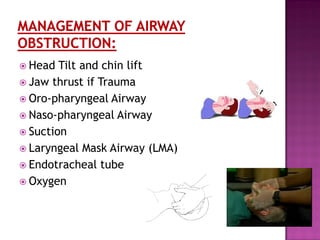
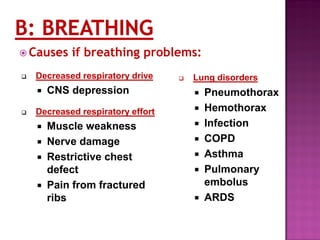
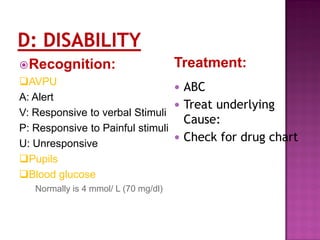
- The ABCDE approach which prioritizes establishing a patient's airway, breathing, circulation, disability level and exposure for examination.
- Techniques for assessing and intervening on airway, breathing and circulation issues including providing oxygen, treating underlying causes, and starting IV fluids.
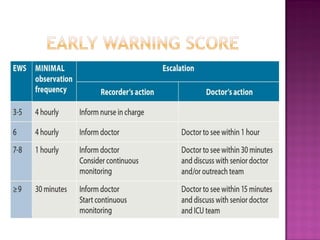
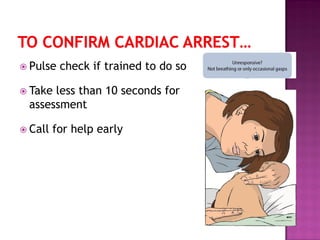
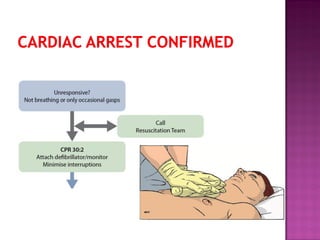
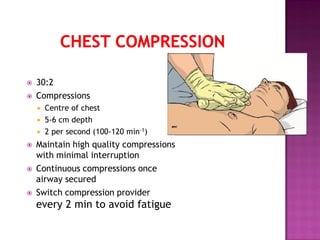
- The importance of continuous reassessment, calling for help early, and following basic life support protocols when indicated to stabilize critically ill patients.