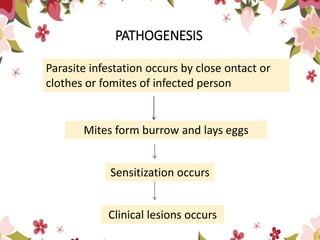
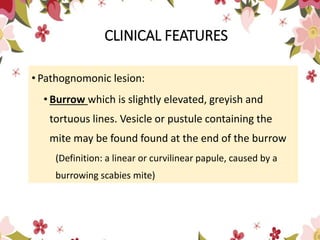
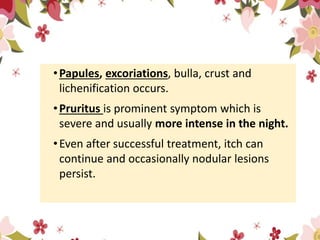
Scabies is a highly contagious skin disease caused by the itch mite Sarcoptes scabiei, spreading through close personal contact and contaminated items. Its clinical features include characteristic burrows, severe itching, and can lead to complications like secondary infections and acute glomerulonephritis. Treatment involves personal hygiene, topical and systemic medications, and ensuring that close contacts are treated simultaneously.