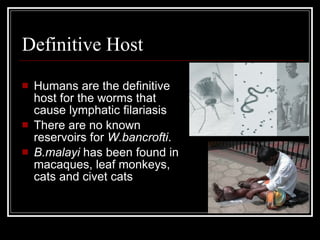
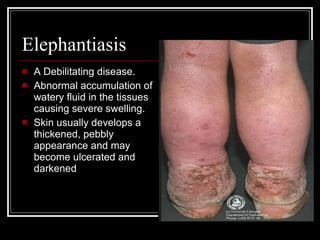
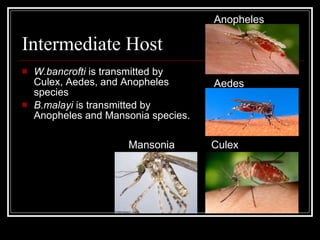
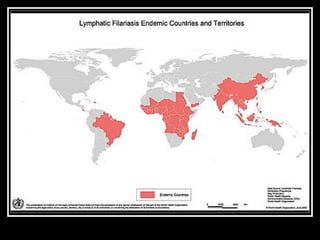
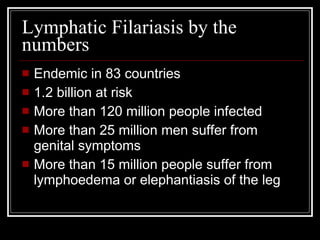
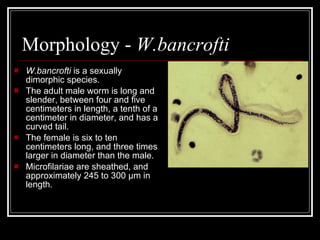
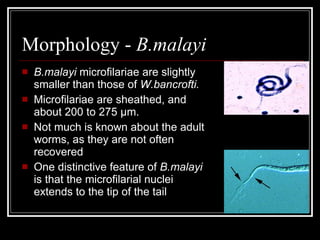
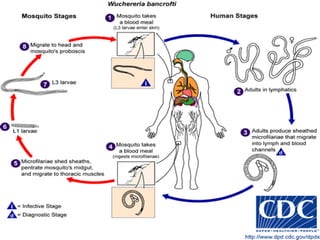
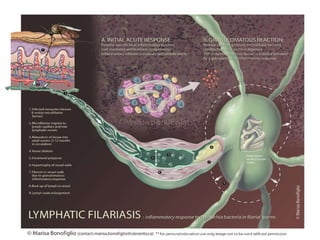
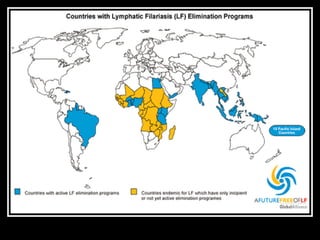
Lymphatic filariasis is caused by parasitic roundworms Wuchereria bancrofti and Brugia malayi, which are transmitted by mosquitoes and can cause elephantiasis. The worms live in the lymphatic system and can cause severe swelling of the limbs and genitals. Over 120 million people are infected globally in tropical areas. Treatment involves drugs to kill the adult worms and microfilariae like diethylcarbamazine, ivermectin and albendazole. Mass drug administration programs combined with mosquito control can eliminate the disease from an area.