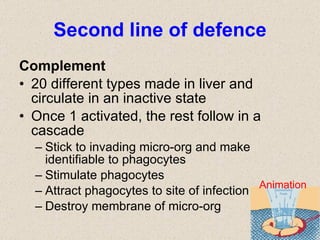
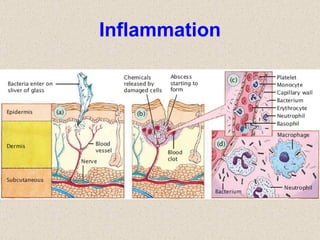
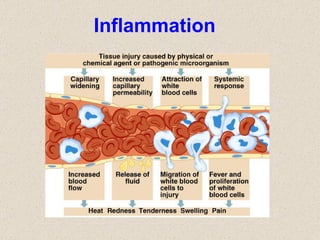
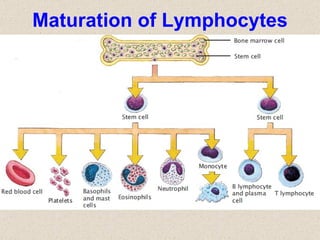
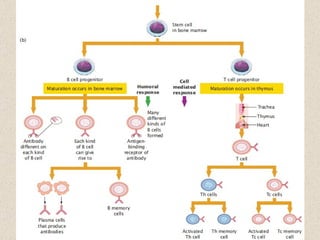
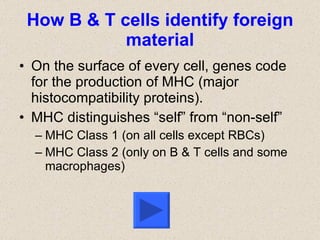
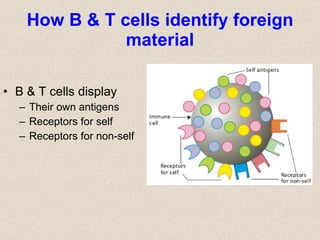
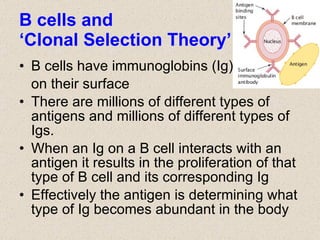
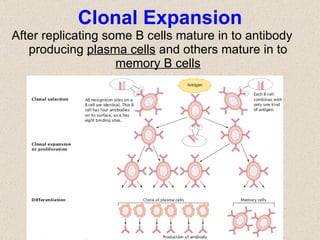
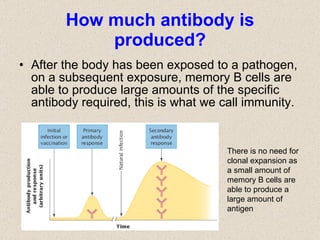
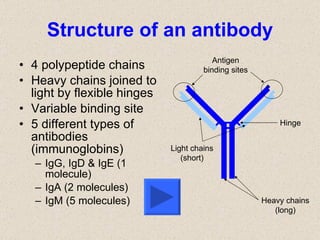
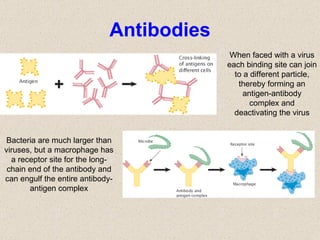
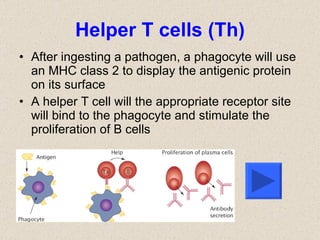
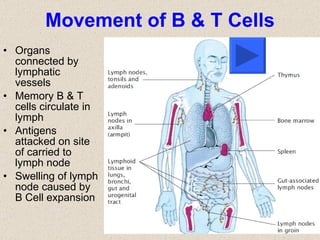
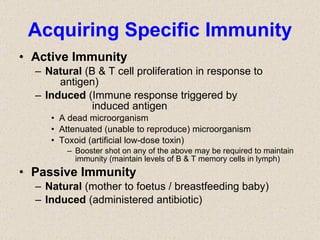
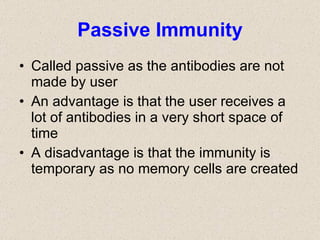
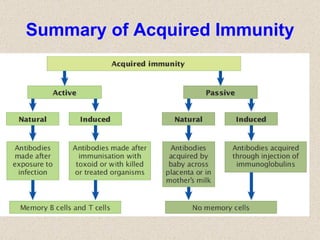
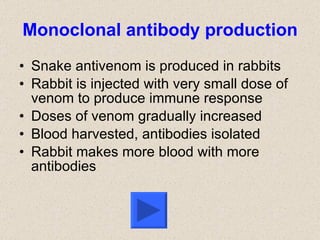
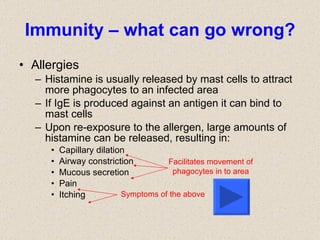
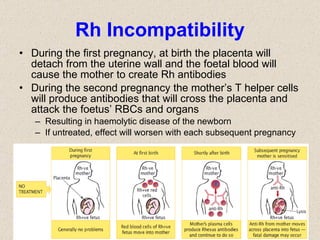
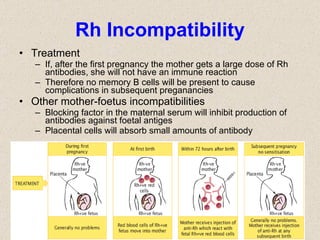
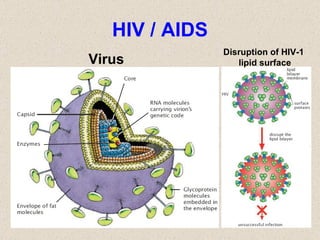
The document discusses the human immune system, including both non-specific (innate) and specific (adaptive) immunity. Non-specific immunity involves physical and chemical barriers that provide a first line of defense against pathogens. If pathogens breach these barriers, white blood cells such as phagocytes, natural killer cells, and the complement system work to destroy invading microorganisms. Specific immunity involves B cells and T cells that can recognize specific pathogens and mount faster and stronger responses upon re-exposure through the production of antibodies and memory cells. The document also discusses immune system disorders like allergies, autoimmune diseases, and immunodeficiencies.