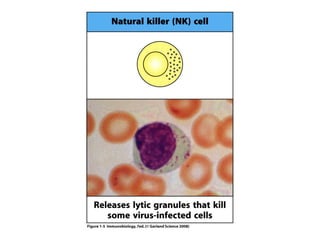
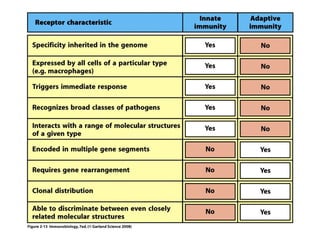
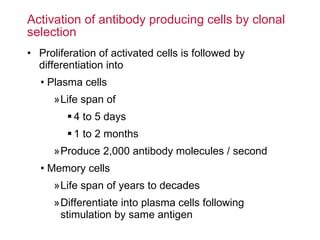
The document provides an introduction to the immune system, discussing both innate and adaptive immunity. It notes that innate immunity provides the first line of defense through physical barriers, complement proteins, and phagocytes. Adaptive immunity involves antigen-specific responses from T and B lymphocytes that result in memory, allowing for faster and stronger secondary responses - the principle behind vaccination.
![Introduction to the Immune system: Lectures 1 and 2 Hugh Brady [email_address] Recommended textbook: Janeway’s Immunobiology (7 th Ed) 2008, Garland Science](https://image.slidesharecdn.com/jimmy-090527094829-phpapp02/85/Jimmy-1-320.jpg)