- Amniotic fluid serves several important roles in fetal development including allowing movement, swallowing, breathing and protecting the fetus.
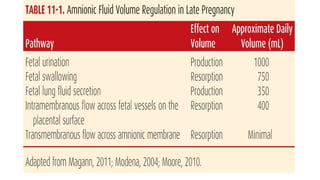
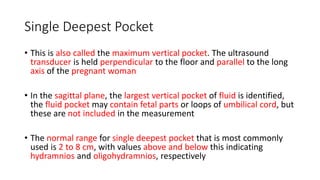
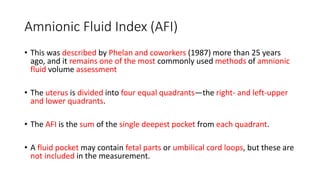
- The normal volume of amniotic fluid increases throughout pregnancy reaching around 800mL by the mid-third trimester. Abnormally low (oligohydramnios) or high (hydramnios) volumes can occur.
- Hydramnios, which complicates 1-2% of pregnancies, has many potential causes including fetal anomalies, diabetes or infections. It can lead to pregnancy complications like cesarean delivery. Oligohydramnios also has various causes like renal abnormalities and medications and is associated with adverse outcomes such as pulmonary hypoplasia