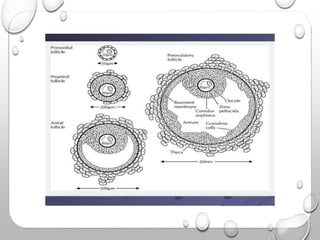
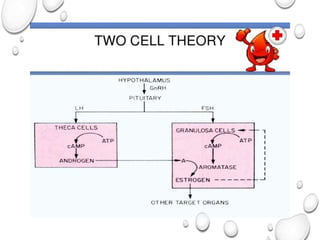
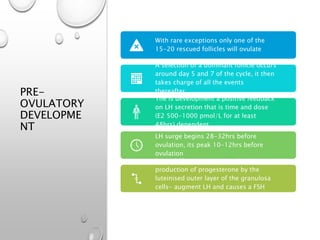
This document summarizes the processes of gametogenesis and ovulation. It discusses folliculogenesis, from primordial follicles to the pre-ovulatory development of the dominant follicle. The luteal phase and corpus luteum formation after ovulation is also described. Finally, it provides an overview of the hormonal regulation of the menstrual cycle by the hypothalamic-pituitary-ovarian axis, and the correlated endometrial changes through the proliferative, secretory and menstrual phases.