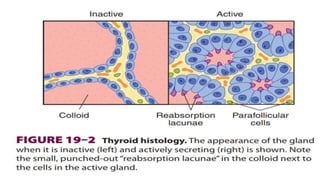
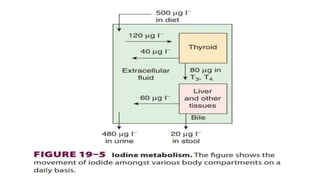
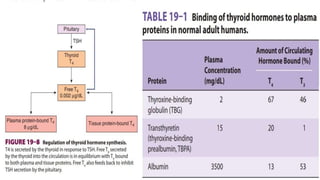
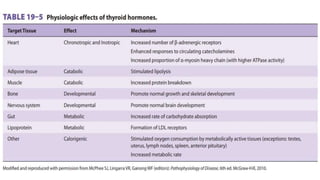
The document summarizes key aspects of the thyroid gland and its functions. It discusses that the thyroid gland secretes thyroid hormones that regulate metabolism and calcium levels. The primary hormones secreted are thyroxine (T4) and triiodothyronine (T3). Iodine is essential for thyroid hormone synthesis and is taken up by the thyroid and kidneys. Within the thyroid, iodine is added to thyroglobulin which is then degraded, releasing T4 and T3 into circulation. Thyroid stimulating hormone (TSH) regulates thyroid function by stimulating hormone synthesis and secretion.