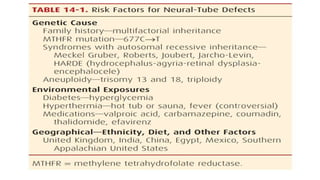
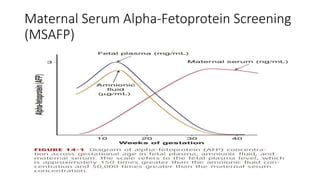
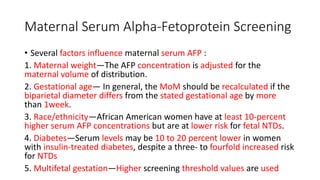
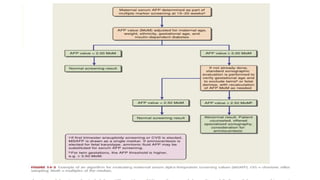
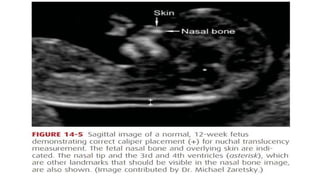
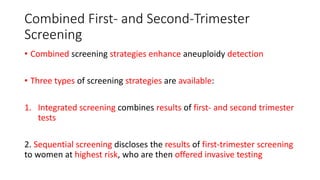
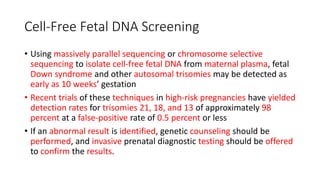
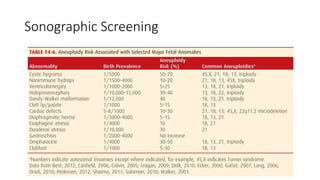
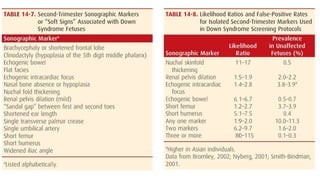
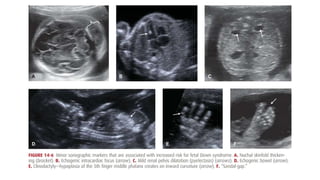
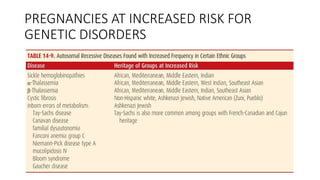
This document provides an overview of prenatal diagnosis. It discusses how major congenital abnormalities are identified in 2-3% of pregnancies and are a leading cause of infant death. Prenatal diagnosis aims to identify fetal malformations, disruptions, and genetic syndromes to improve counseling. Structural abnormalities can develop through malformation, deformation, or disruption. Neural tube defects are among the most common birth defects. Maternal serum screening for alpha-fetoprotein is an established screening test for neural tube defects. Advances in screening include first trimester screening using nuchal translucency and serum markers, as well as cell-free DNA screening. Sonographic screening can identify soft markers and structural abnormalities. Pregnancies at