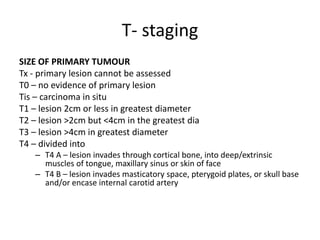
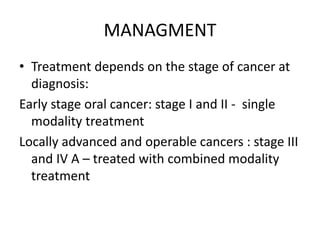
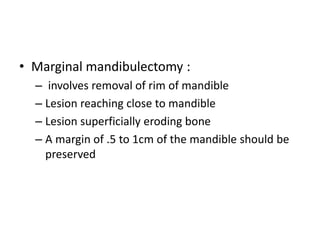
The document discusses TNM staging for oral cancer. TNM staging classifies tumors based on the size of the primary tumor (T stage), presence of lymph node metastasis (N stage), and distant metastasis (M stage). Treatment depends on the cancer stage - early stage cancers are generally treated with single modality like surgery or radiation, while locally advanced or operable stage III/IV cancers receive combined modality treatment like surgery followed by radiation and/or chemotherapy. Management of neck lymph nodes also depends on whether they are clinically positive or negative.