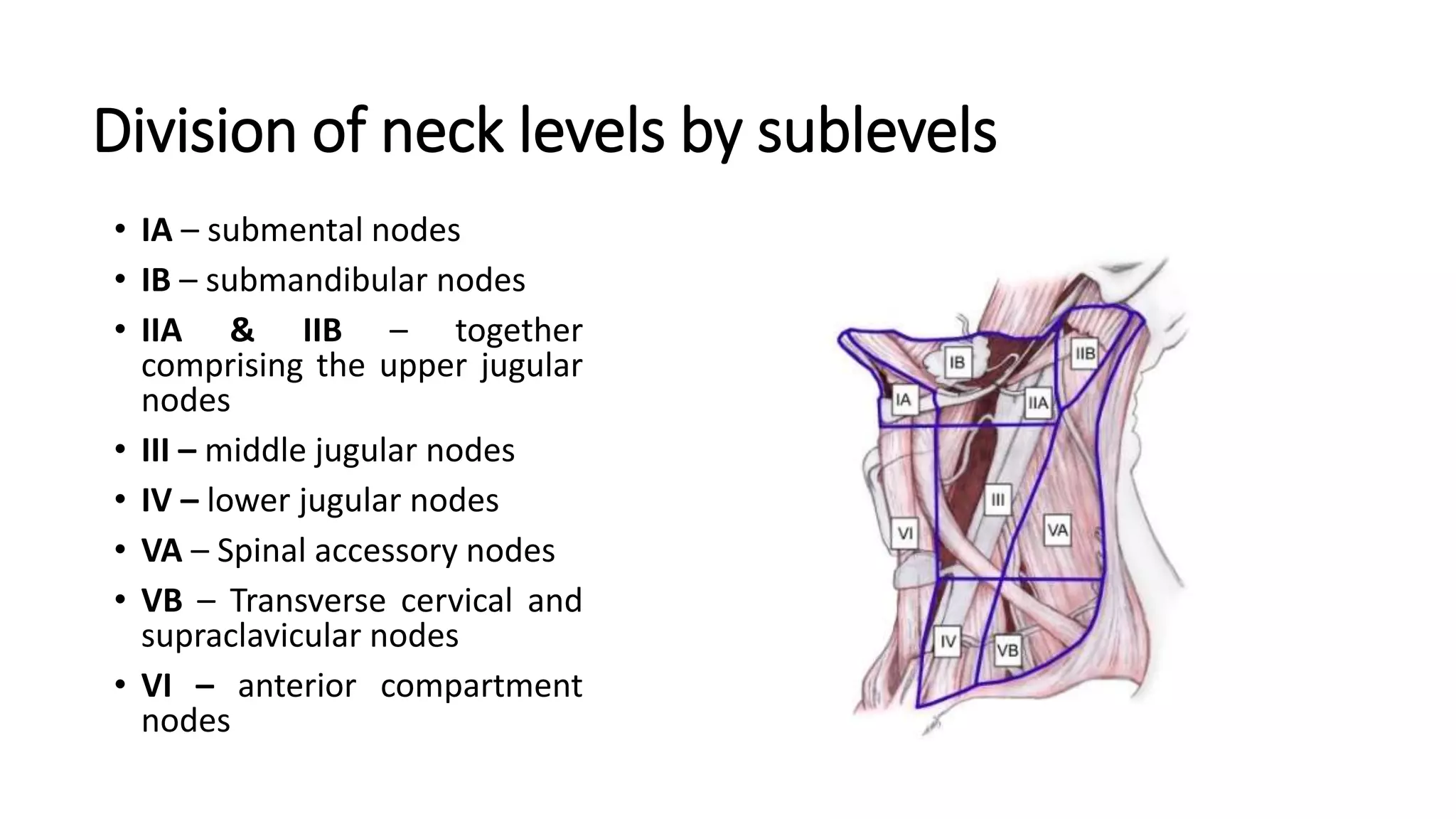
This document discusses neck dissection procedures for treating head and neck cancers. It covers:
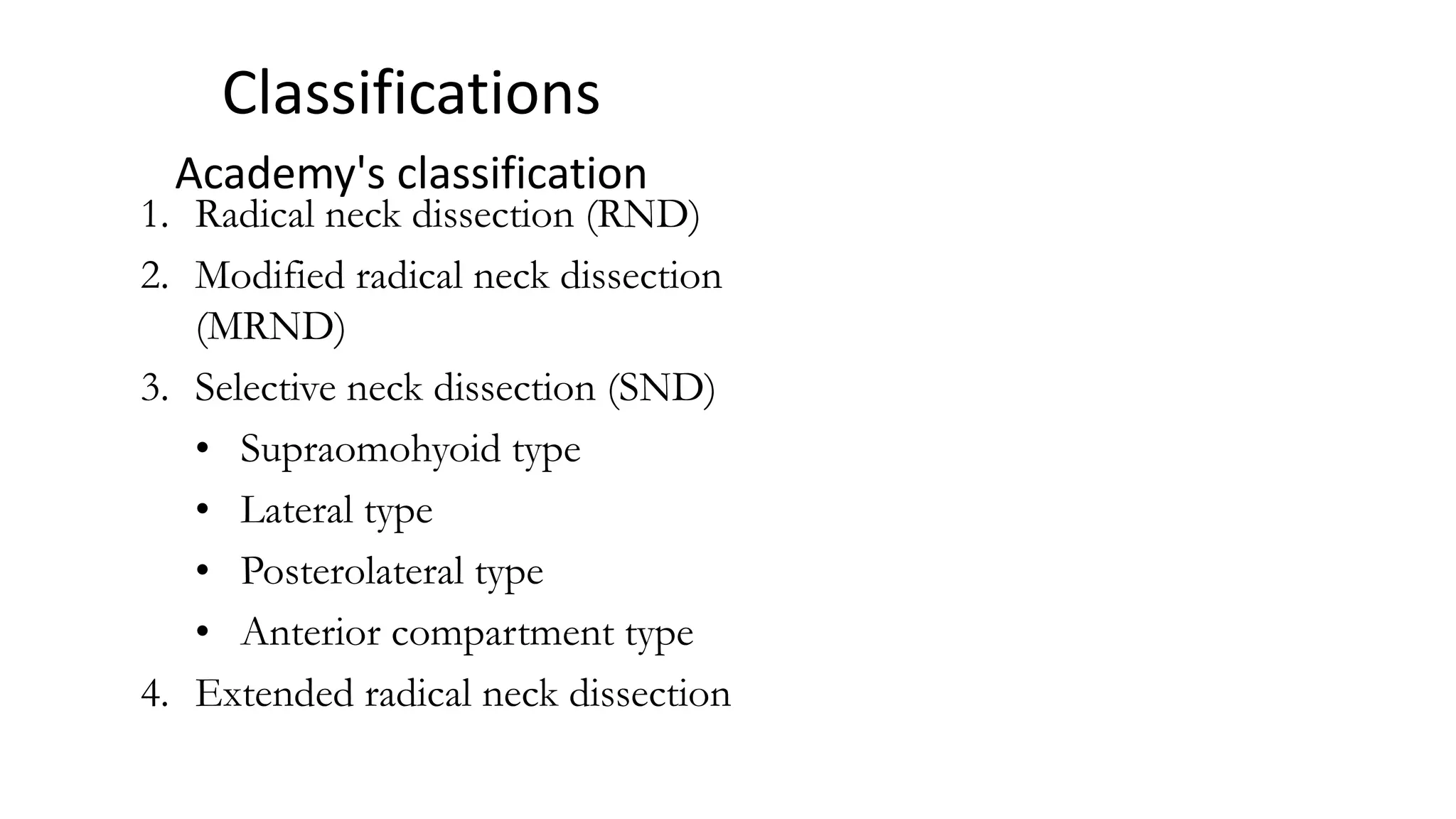
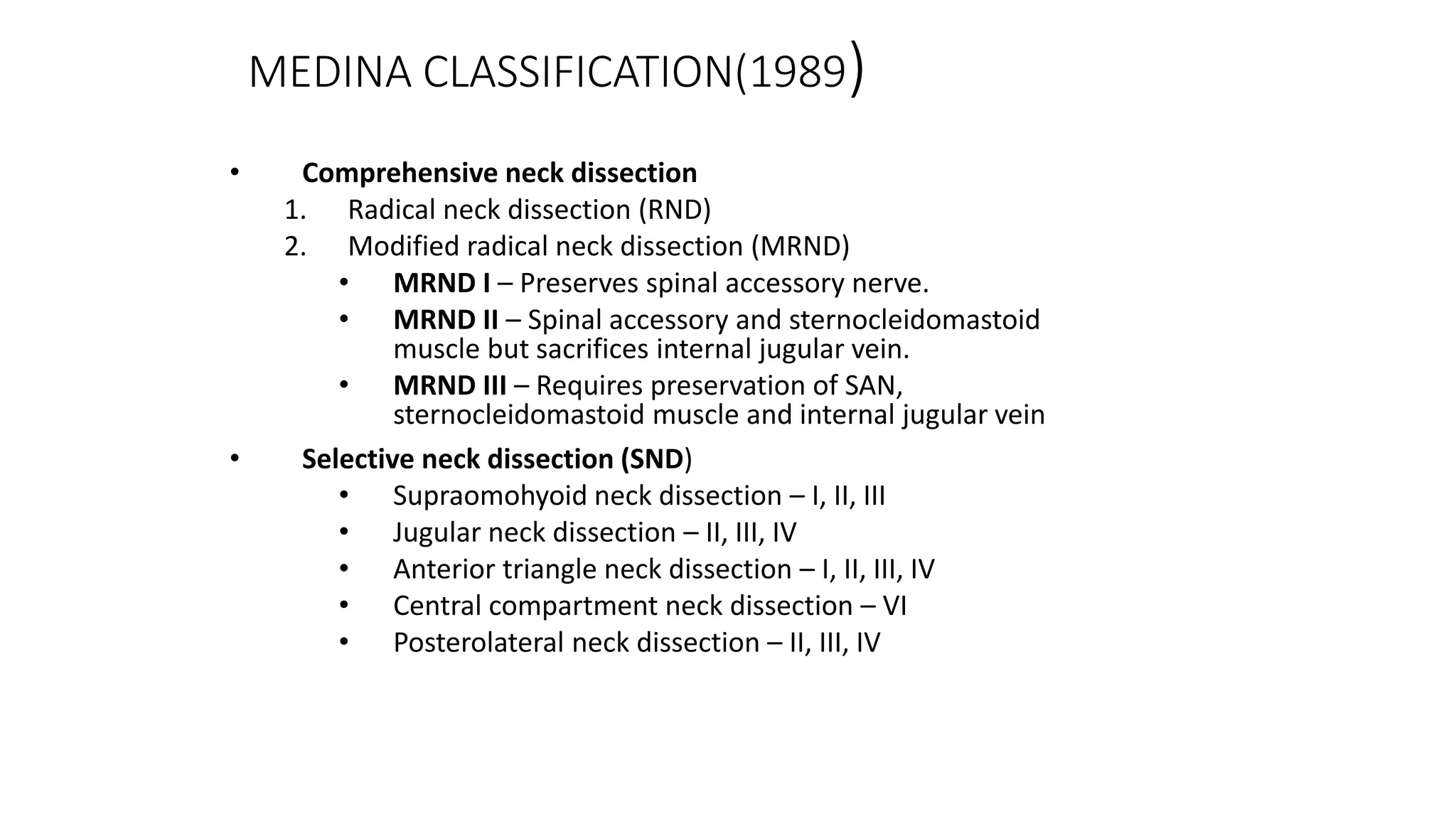
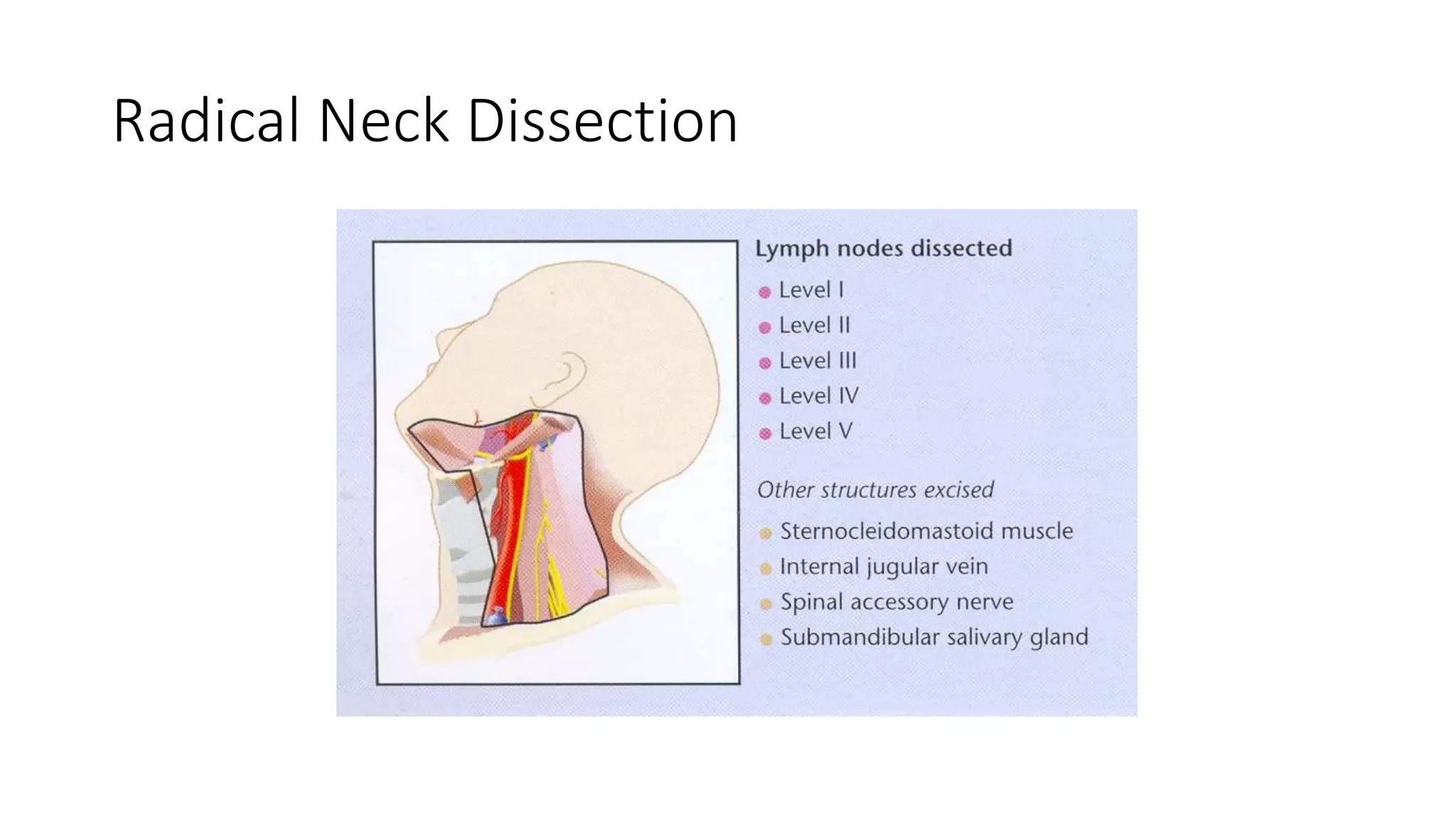
1. The types of neck dissections including radical neck dissection (RND), modified radical neck dissection (MRND), and selective neck dissection (SND). RND removes the highest number of lymph nodes while SND removes the fewest.
2. Factors that influence the risk of lymph node metastasis including primary tumor site, size, and histology. The first echelon lymph nodes that drain different primary sites are also described.
3. Staging of neck cancers using the TNM system and guidelines for indications of different neck dissection procedures based on tumor staging.