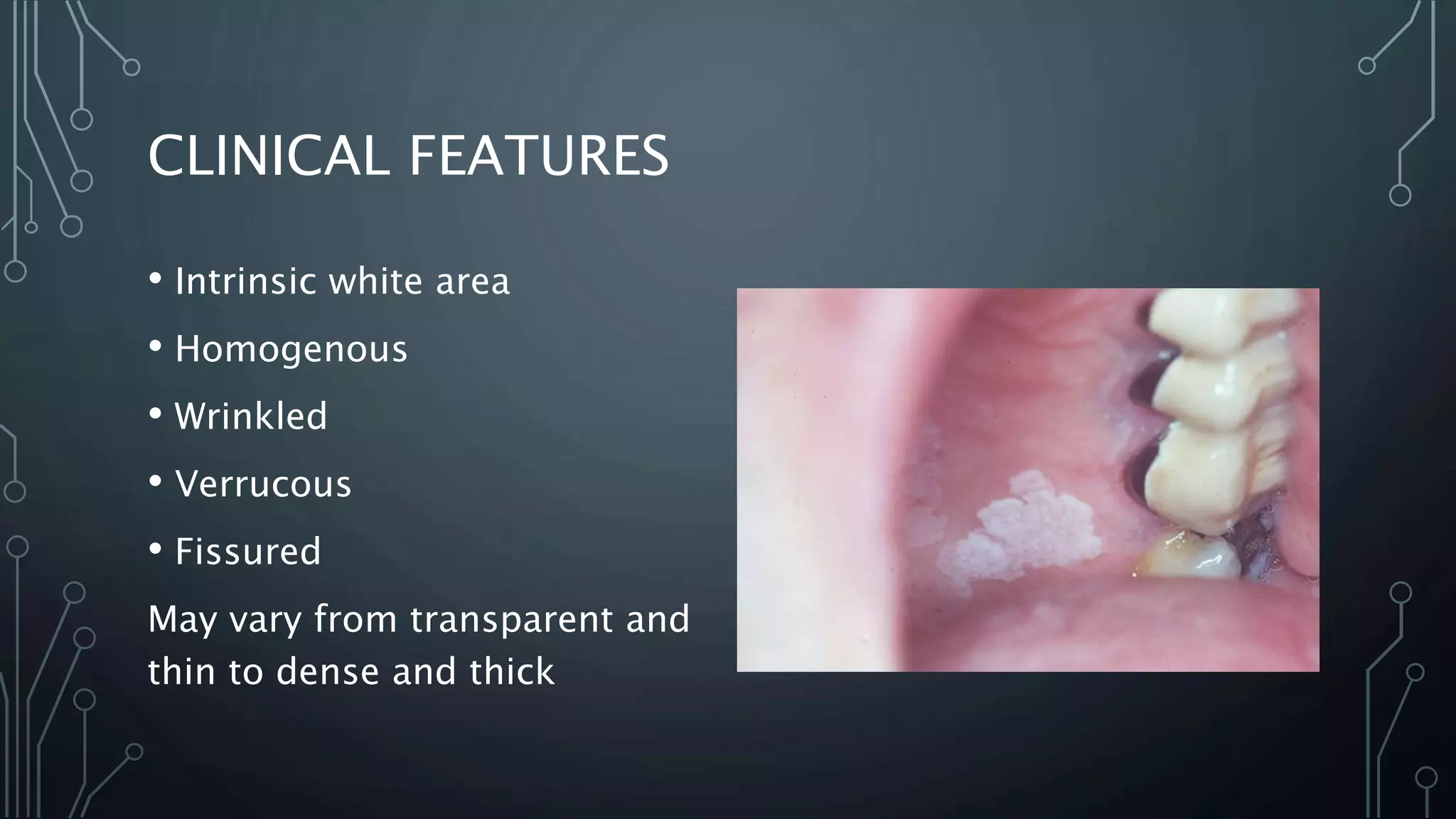
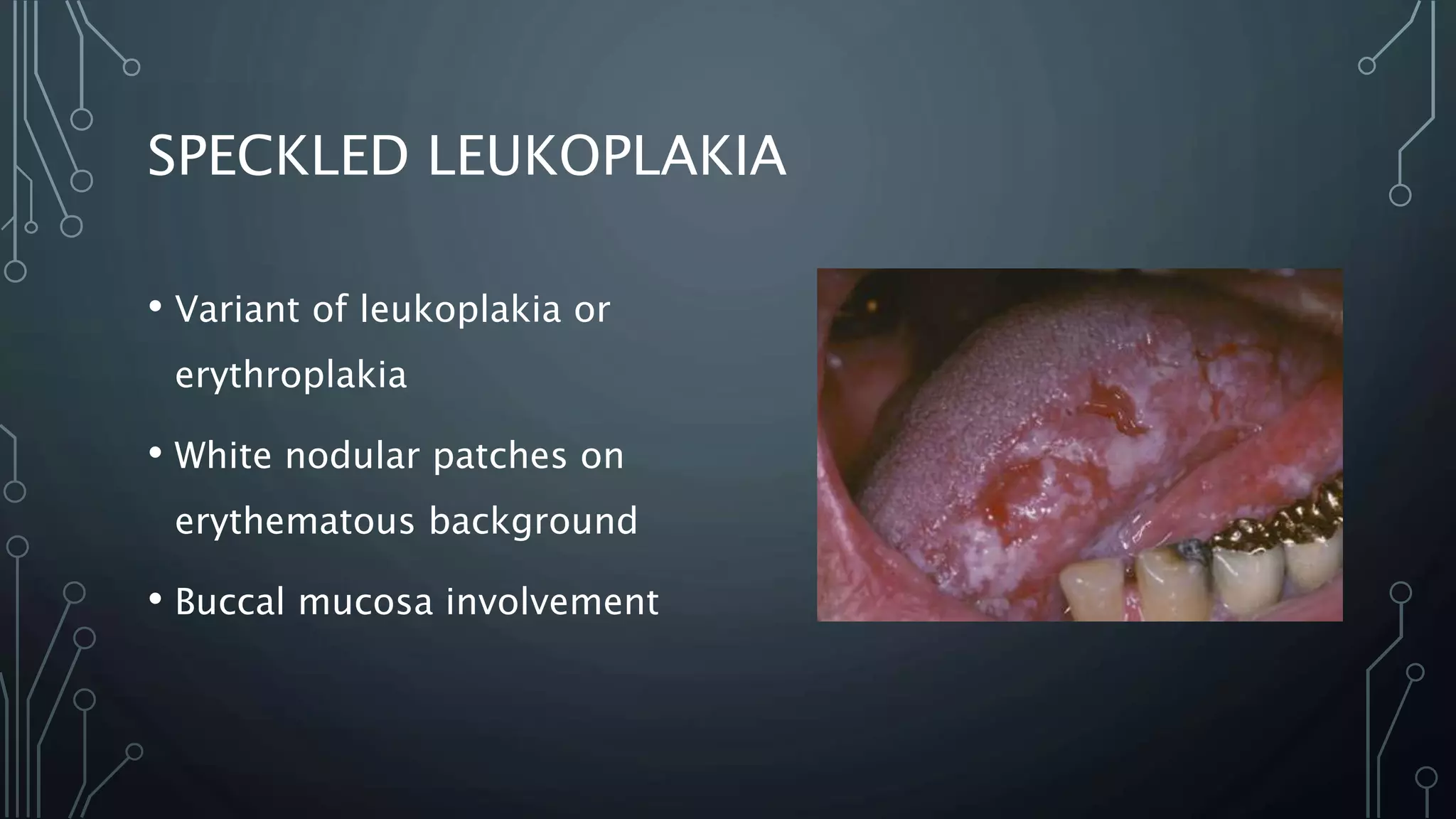
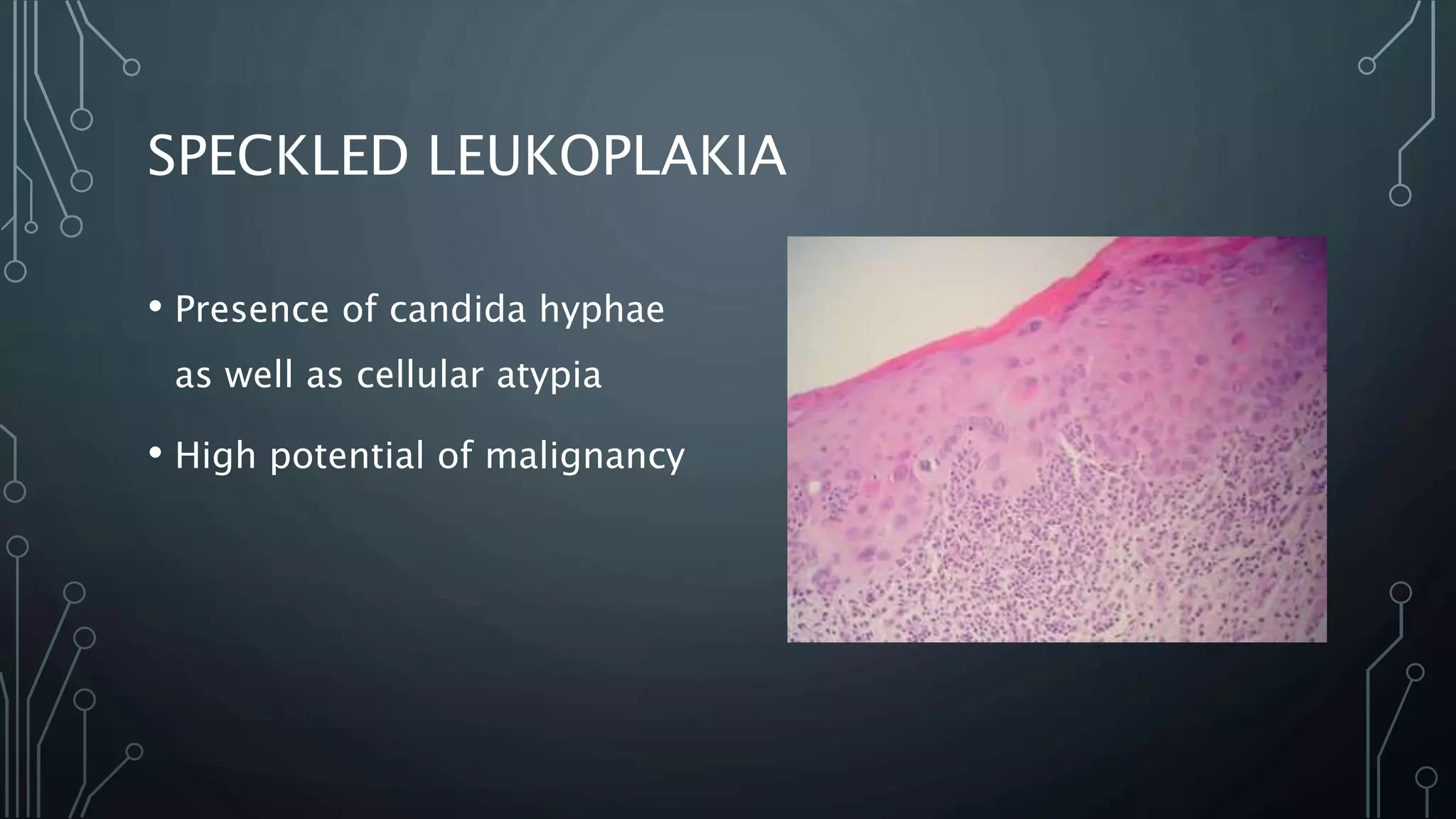
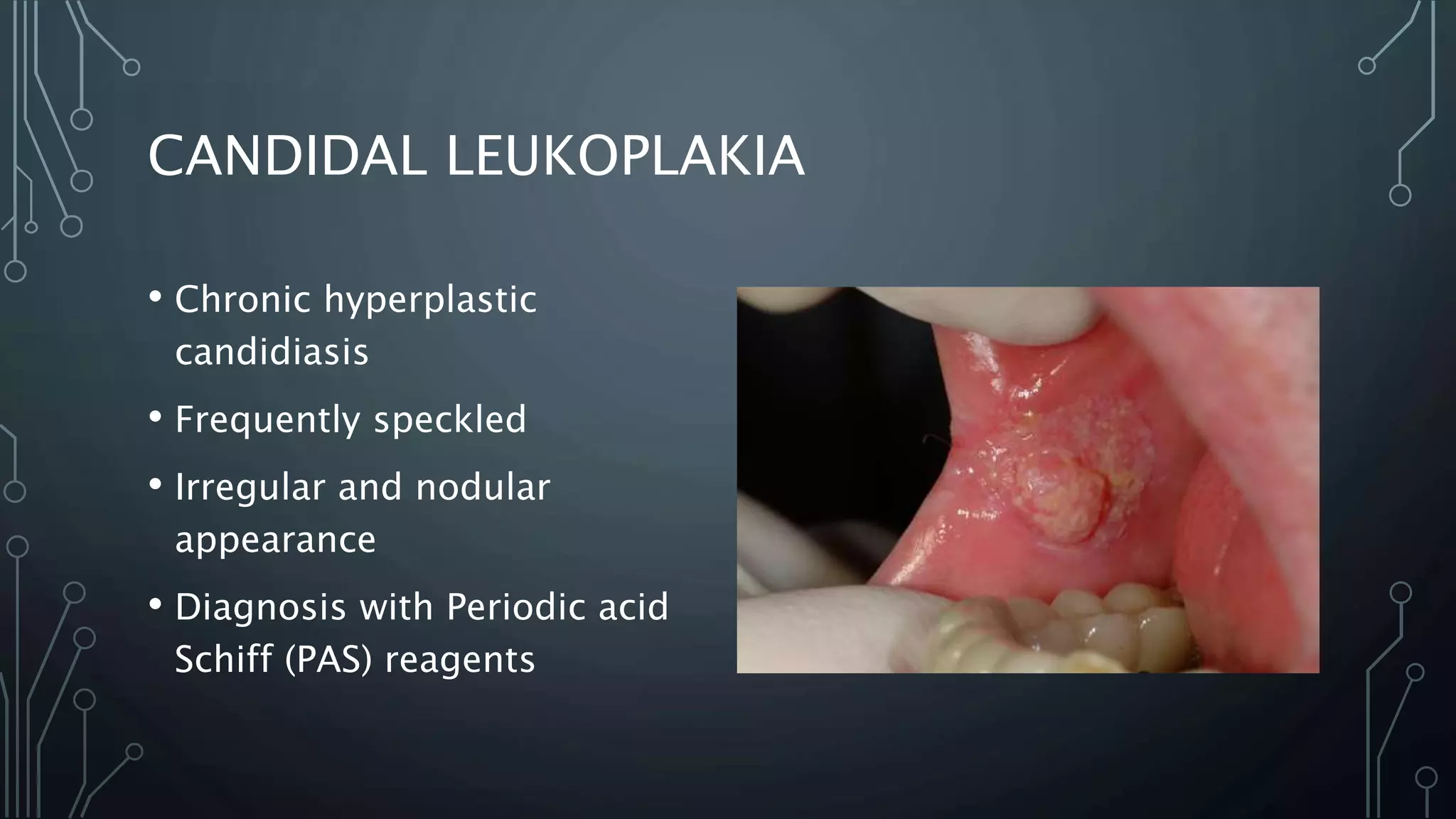
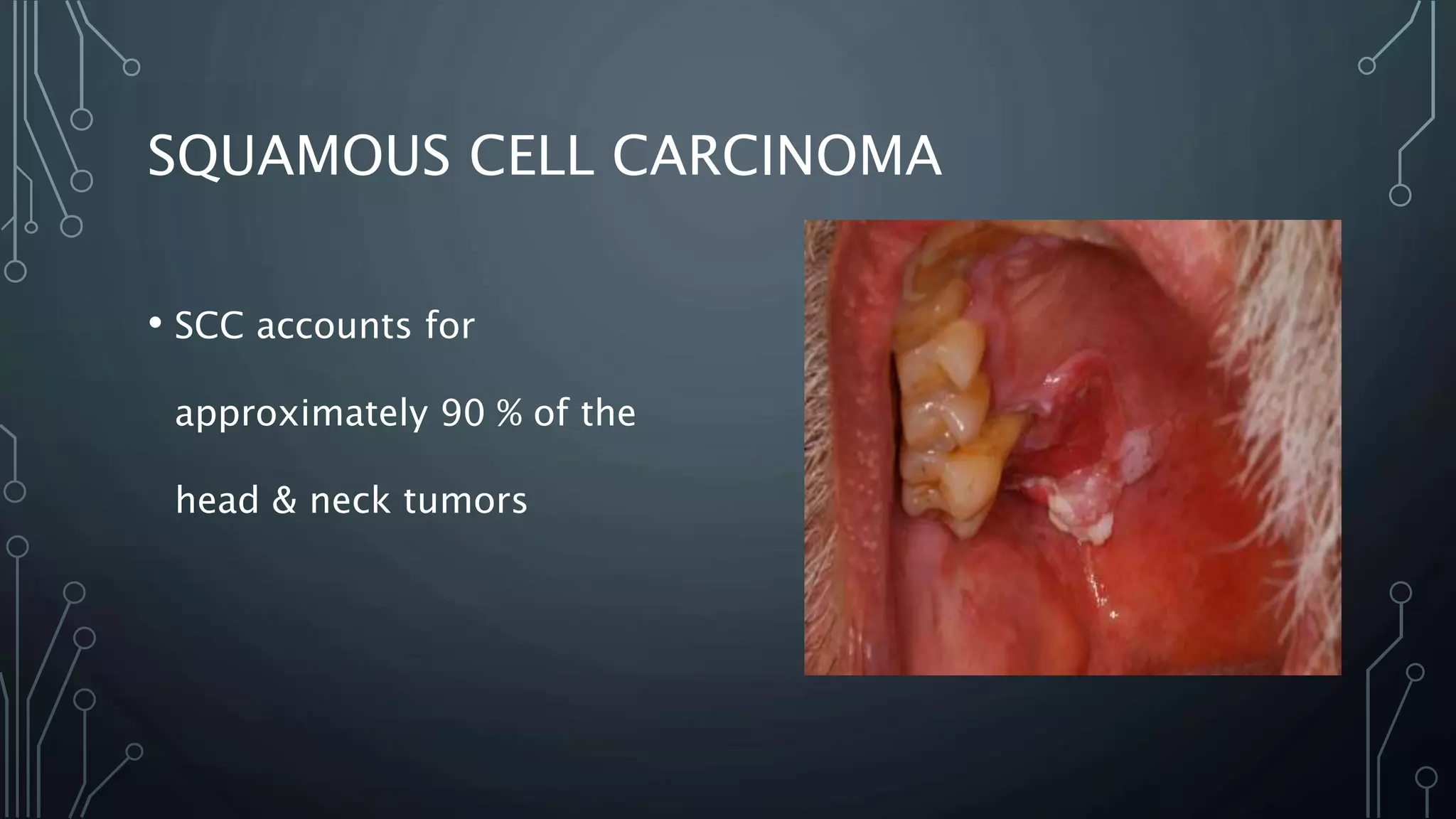
This document discusses precancerous lesions and conditions of the oral cavity. It defines precancerous lesions as morphologically altered tissues with a higher risk of developing cancer, and precancerous conditions as generalized states associated with significantly increased cancer risk. Examples of precancerous lesions include leukoplakia, erythroplakia, and speckled leukoplakia. Oral submucous fibrosis and sideropenic dysphagia are examples of precancerous conditions. Risk factors for oral cancer development from these lesions include tobacco, alcohol, infections and nutritional deficiencies. Screening, early identification and treatment can help prevent progression to oral squamous cell carcinoma.