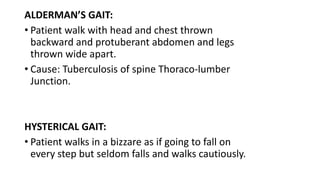
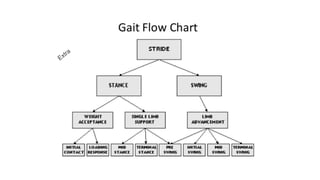
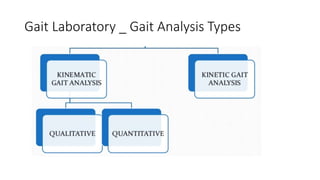
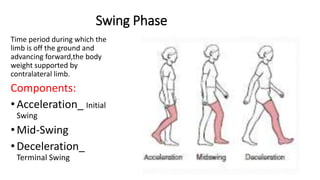
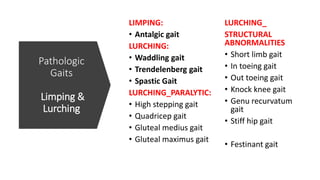
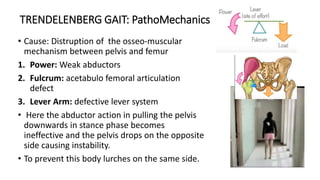
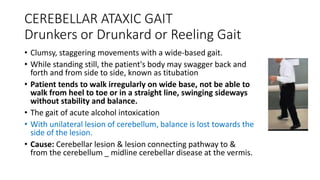
The document discusses gait disorders, their classifications, and analysis techniques, including video-assisted observational gait analysis (VAOGA). It outlines the types and causes of gait disorders, emphasizing the importance of proper assessment to improve mobility and prevent falls, particularly in the elderly. The document also details various gait patterns associated with different conditions, such as cerebral palsy and other pathological causes.

![GAIT DISORDER_MAJOR REASONS:
• Deformities
• Weakness / Loss of motor control
• Pain: Inflamatory / infective disorder
• Multifactorial [common & Complex
with advancing age]
Prevelence increases with ageing
population and increasing morbidity
index
Look when he bears weight on left leg](https://image.slidesharecdn.com/4anisgaitdisorders-200927092356/85/4_anisbhatti-gait-disorders-4-320.jpg)

![• Careful history taking &
examination focussed on:
oGait pattern
oPhysical examination
oNeurological assesment
oOrthopaedic evaluation
oGait Analysis [VAOGA]
• Objectives to
improve
oMobility
oIndependence,
oPrevent falls
oDetect underlying
causes
Assesment & Evaluation:
Two basic steps in the categorization of gait disorders and guideline for ancillary investigations and
therapeutic interventions includes:.](https://image.slidesharecdn.com/4anisgaitdisorders-200927092356/85/4_anisbhatti-gait-disorders-6-320.jpg)

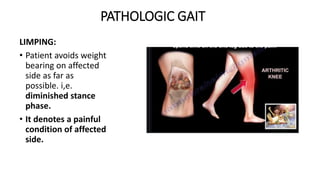

![ANTALGIC GAIT_ Limp
• Gait pattern in which stance
phase on affected side is
shortened due to pain in the
weight bearing limb.
• There is corresponding increase
in stance phase on unaffected
side
• Common causes:
Osteoarthritis [Coxalgia], LCPD,
SCFE,Fractures, tendinitis](https://image.slidesharecdn.com/4anisgaitdisorders-200927092356/85/4_anisbhatti-gait-disorders-40-320.jpg)





![Type II
True Equinus
hemiplegic gait.
(a): Right-sided
hemiplegia with ankle
equinus in stance [AP view].
(b): Right-sided
hemiplegia with ankle
equinus in stance [Lat view]
Equinus With
Recurvatu](https://image.slidesharecdn.com/4anisgaitdisorders-200927092356/85/4_anisbhatti-gait-disorders-64-320.jpg)
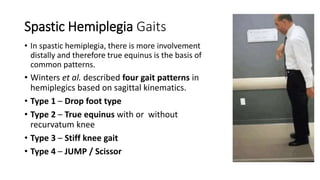
![Spastic Hemiplegia Gaits
• Type 3 – Stiff knee gait: Rectus Femoris over active
in Swing phase
• Type 4 – JUMP [Common in diplegics]
In sagittal plane, the ankle is in equinus, knee in
flexion, hip in flexion and anterior pelvic tilt is
present.
In coronal plane, there is hip adduction and
internal rotation.](https://image.slidesharecdn.com/4anisgaitdisorders-200927092356/85/4_anisbhatti-gait-disorders-65-320.jpg)
![Apparent Equinus
[Dynamic Equinus]
• Hip flexion
• Knee flexion
• Ankle neutral..
plantigrade
Pic Courtesy: Prof. Sharaf Ibrahim, Malaysia](https://image.slidesharecdn.com/4anisgaitdisorders-200927092356/85/4_anisbhatti-gait-disorders-72-320.jpg)
![Cerebelar_ Ataxia
• Lack of Balance
• Uncoordinated Movement
• Dysmetria [Fig.A]
• Wide base _Sway as he walks.
[Fig B]
• Pes Valgus (flexible) common](https://image.slidesharecdn.com/4anisgaitdisorders-200927092356/85/4_anisbhatti-gait-disorders-77-320.jpg)
![CHOREIFORM_ Hyperkinetic GAIT:
• The patient will be having chorea
[Irregular, Jerky, Involuntary
movements] more in upper limbs &
has a unstable gait.
• Walking may accentuate their
baseline movement disorder.
• Seen in patients having
extrapyramidal symptoms
• Cause: Basal ganglia disorders including
Sydenham's chorea, Huntington's Disease and
other forms of chorea, athetosis or dystonia.](https://image.slidesharecdn.com/4anisgaitdisorders-200927092356/85/4_anisbhatti-gait-disorders-78-320.jpg)