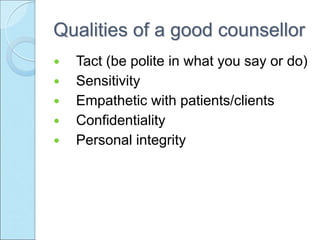
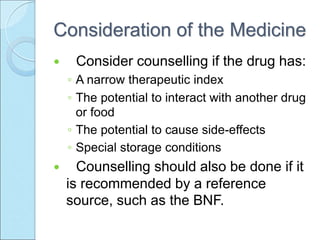
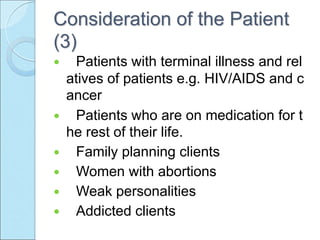
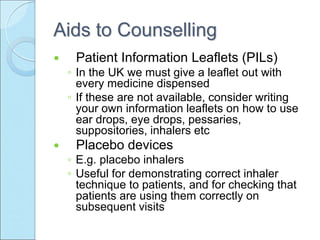
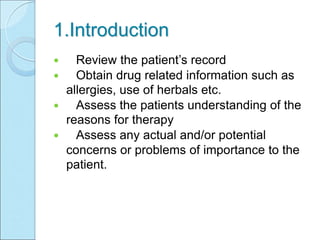
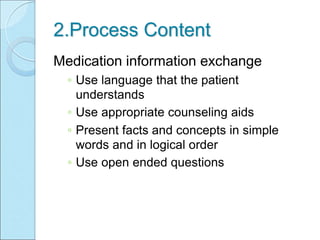
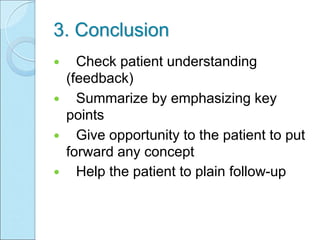
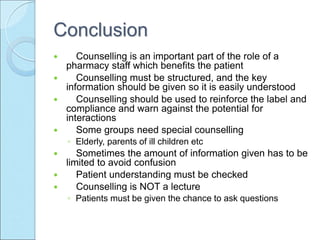
Counseling skills are important for pharmacy staff to effectively communicate medication instructions to patients. The counseling process involves introducing the medication, exchanging key information about proper use, and concluding by checking patient understanding. Staff should consider qualities like knowledge, communication skills, and empathy when counseling. Opportunities to counsel include when dispensing medications. The goals are to improve patient adherence and outcomes by ensuring they understand how and why to take their medications correctly.