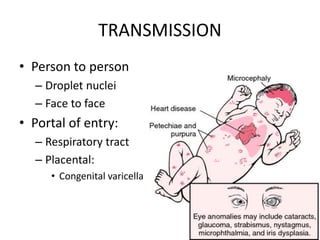
1. Chickenpox (Varicella) is caused by the varicella-zoster virus and results in a characteristic rash with superficial vesicles in crops over the body.
2. It is highly contagious from 1-2 days before the rash appears until the lesions crust over, about 4-5 days after rash onset.
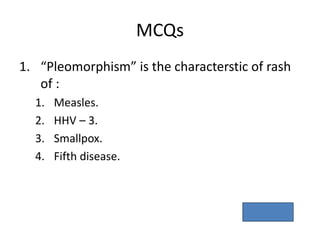
3. The rash progresses quickly through stages from macule to papule to vesicle to scab over 4-7 days, with new crops appearing as older ones resolve, resulting in a pleomorphic rash.