This document summarizes tuberculosis (TB), including its cause, affected organs, history, epidemiology, diagnosis, treatment, and prevention. Key points include:
- TB is caused by the bacterium Mycobacterium tuberculosis, which most commonly affects the lungs.
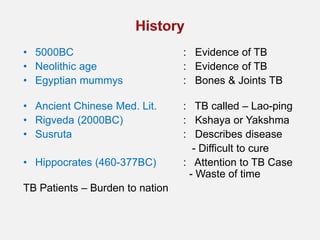
- TB has been documented as far back as 5000 BC in ancient Egypt and China. Major advances in understanding and treating TB came in the late 19th/early 20th centuries.
- India has the highest global TB burden, with over 2 million new cases annually. Diagnosis involves sputum microscopy and culture, while treatment requires a multi-drug regimen over 6-24 months.
- Prevention involves the BCG vaccine and identifying latent