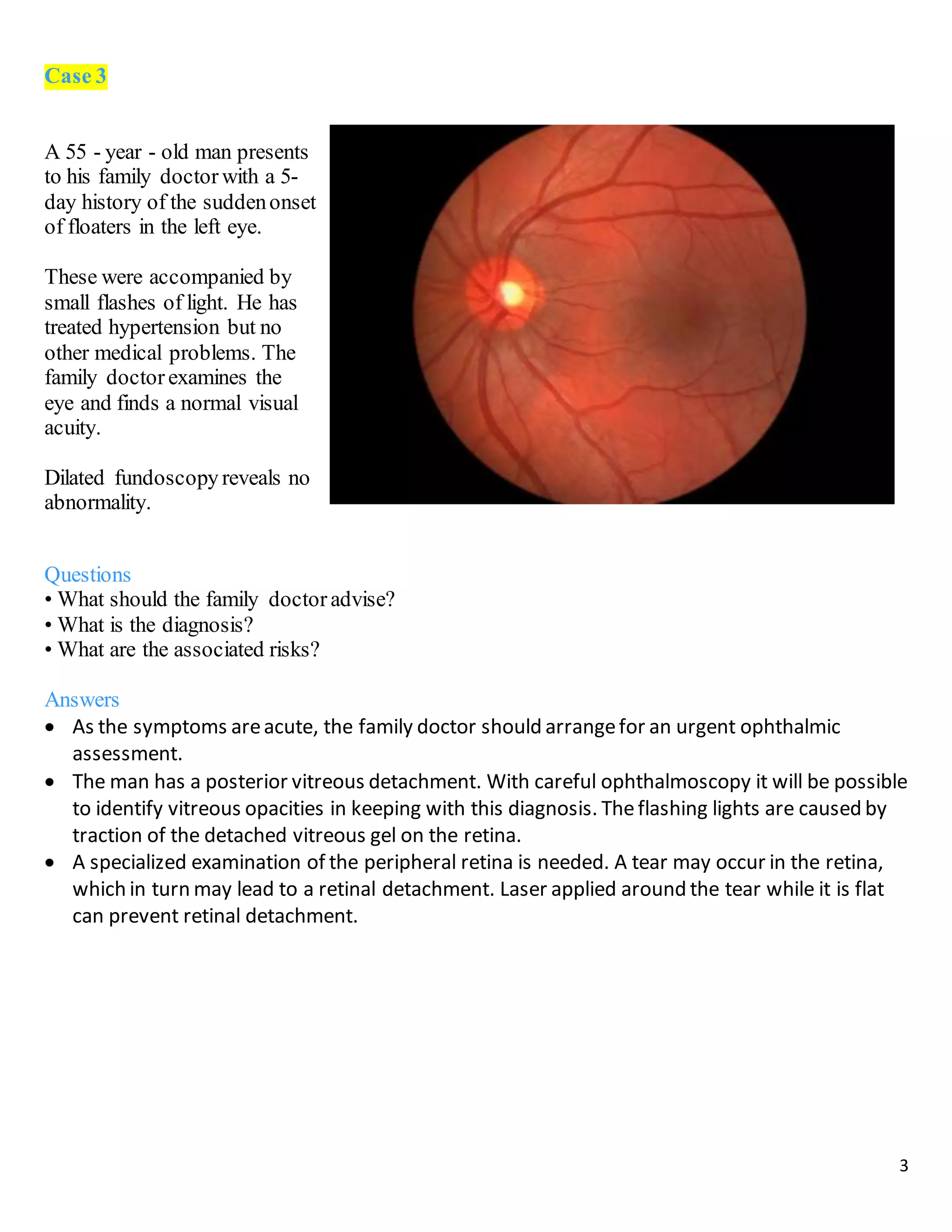
The document describes 10 medical cases involving patients presenting with various eye symptoms. Case 1 involves a 70-year-old woman with sudden vision loss, headache, and jaw pain, likely due to giant cell arteritis. Case 2 involves a 40-year-old man with a drooping eyelid and double vision, likely caused by a third nerve palsy from an aneurysm. Case 3 involves a 55-year-old man with floaters and flashes, diagnosed with a posterior vitreous detachment.