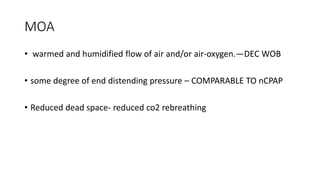
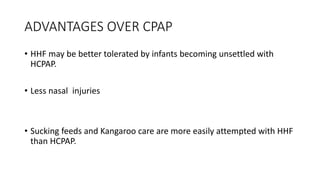
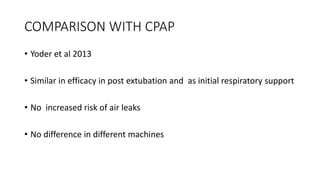
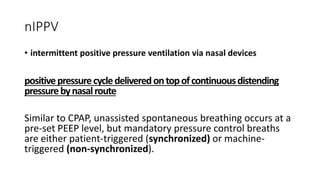
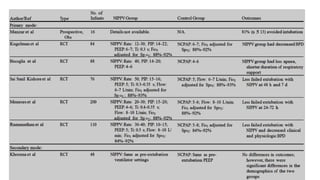
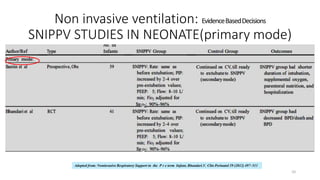
The document discusses non-invasive ventilation (NIV) techniques for neonates, particularly nasal intermittent positive pressure ventilation (NIPPV) and its advantages over nasal continuous positive airway pressure (NCPAP). It highlights studies indicating lower extubation failure rates and better outcomes for apnea of prematurity with NIPPV, and provides guidelines for the application and settings of NIPPV in primary and secondary modes. Additionally, it covers the effectiveness of high-flow nasal cannula and other NIV modes, emphasizing the need for further research on their comparative efficacy.
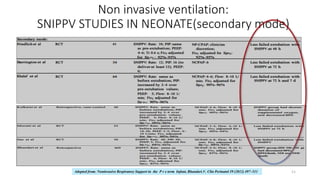
![Non invasive ventilation: Evidence Based
Decisions : NIPPV VS NCPAP
12
EXTUBATION FAILURE RATE:NIPPV VS NCPAP
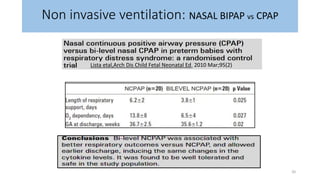
Nasal Intermittent Positive Pressure Ventilation versus Nasal Continuos Positive Airway Pressure in Neonates: A
Systematic Review and Meta-analysis: Tang et al, Indian pediatrics,2012
Five papers reported the rate of extubation failure of NIPPV
versus nCPAP following ETT and mechanical ventilation.
Meta-analysis showed that the rate of extubation
failure of NIPPV was significantly lower than that of
nCPAP [OR=0.15 (95% CI: 0.08 0.31)]; P<0.001.](https://image.slidesharecdn.com/niv2-170214170708/85/NON-INVASIVE-VENTILATION-IN-NEONATES-PART-2-12-320.jpg)
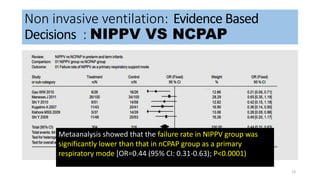
![Non invasive ventilation: Evidence Based
Decisions : NIPPV VS NCPAP
14
META-ANALYSIS OF SECONDARY OUTCOMES BETWEEN NIPPV AND NCPAP GROUPS
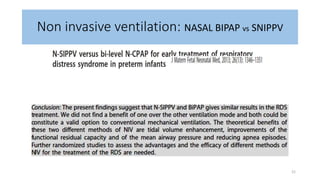
Nasal Intermittent Positive Pressure Ventilation versus Nasal Continuos Positive Airway Pressure in Neonates: A
Systematic Review and Meta-analysis: Tang et al, Indian pediatrics,2012
• FINAL OUTCOME (DEATH AND/OR BPD): NIPPV was significantly better than that of nCPAP as a primary
respiratory mode [OR=0.57 (95% CI: 0.37-0.88); P=0.01]
• APNEA OF PREMATURITY: NIPPV showed a statistically lower rate of apnea (episodes per hour) as compared
with nCPAP group [WMD=-0.48 (95%CI:-0.58-0.37; P<0.001]
• DURATION OF HOSPITALIZATION : (primary respiratory mode /extubation mode) : No significant difference in
duration of hospitalization between NIPPV and nCPAP group [WMD=-0.51 (95%CI:-5.62-4.61;
• INCIDENCE OF BPD : NIPPV led to a marginally significant reduction in the incidence of BPD as compared
with nCPAP. [OR(95%CI)=0.39-1.00,P=0.05]
• incidence of IVH, PVL, ROP, PDA, Pneumothorax or air leak, abdominal distention, necrotizing enterocolitis :
no significant differences](https://image.slidesharecdn.com/niv2-170214170708/85/NON-INVASIVE-VENTILATION-IN-NEONATES-PART-2-14-320.jpg)