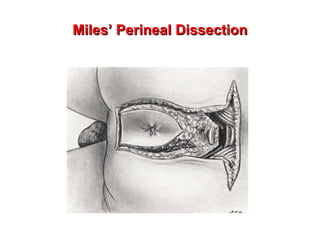
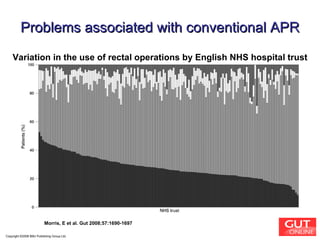
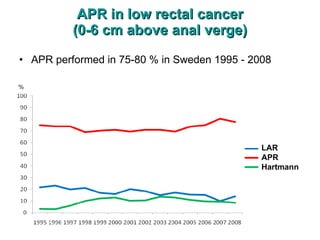
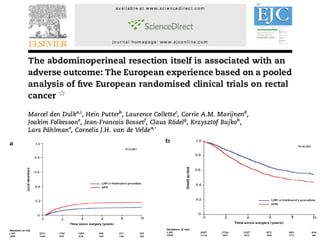
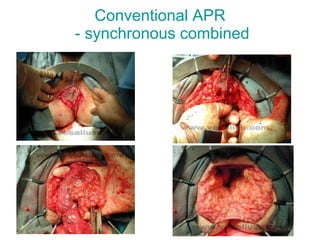
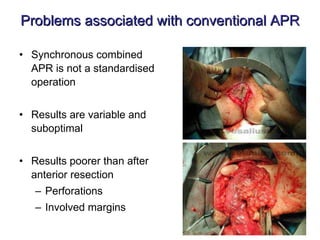
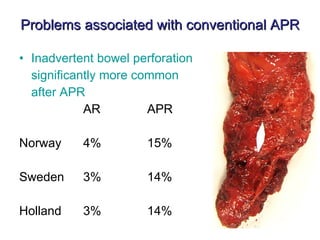
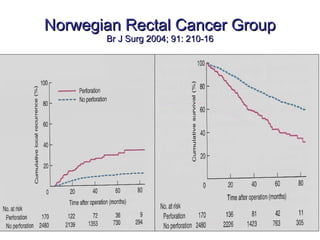
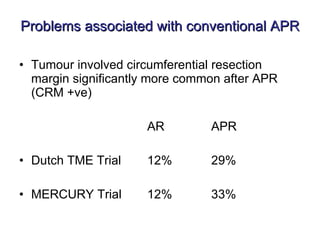
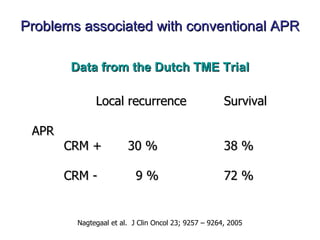
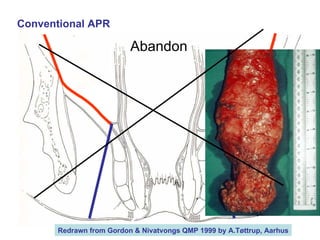
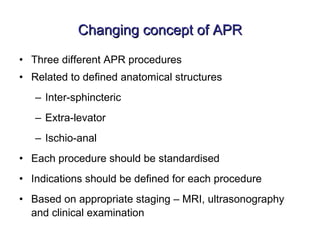
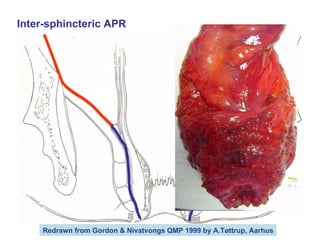
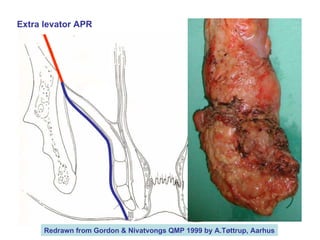
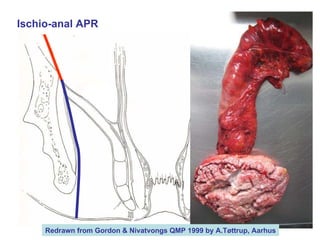
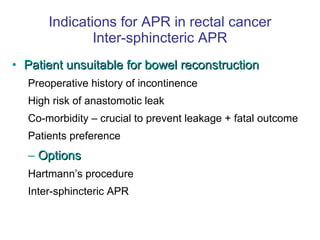
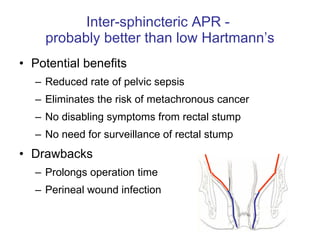
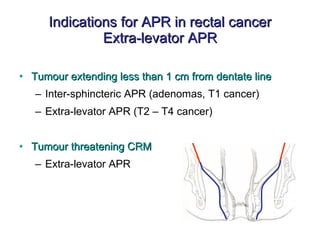
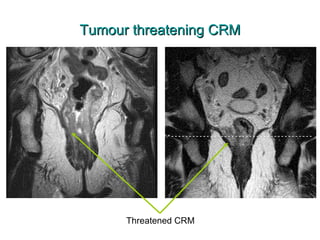
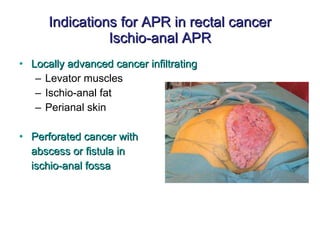
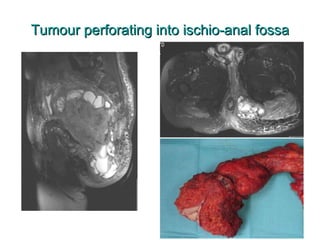
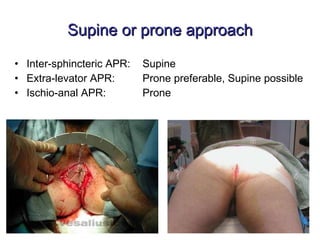
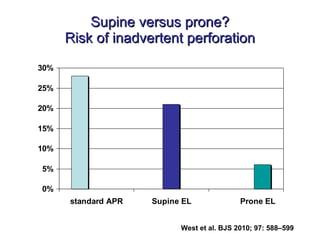
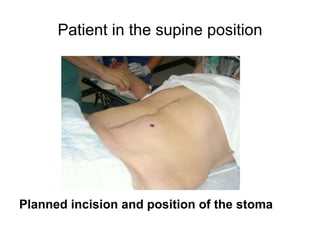
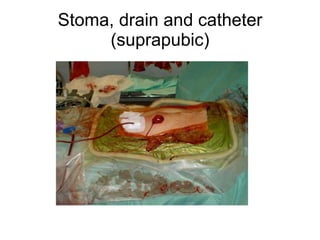
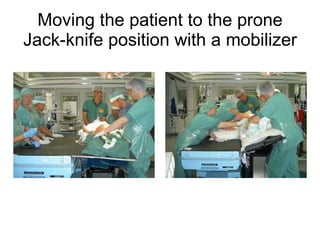
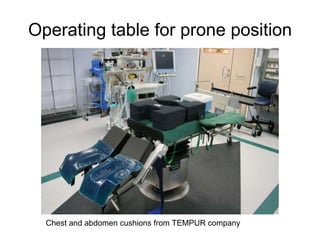
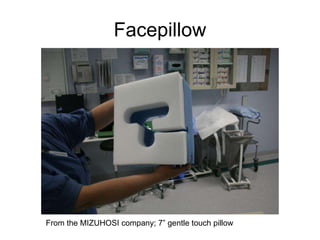
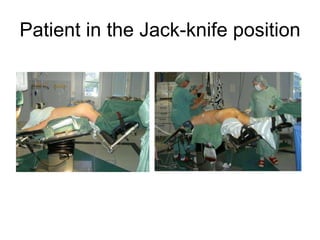
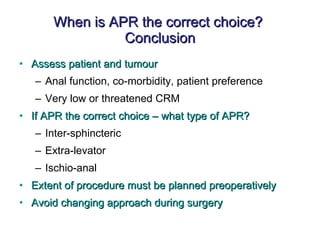
The document discusses different techniques for performing an abdominoperineal resection (APR) for rectal cancer. It outlines problems with the conventional synchronous APR approach and proposes changing to standardized inter-sphincteric, extra-levator, or ischio-anal APR depending on tumor location. Each technique is defined by its relationship to anatomical structures. Indications, advantages, and positioning considerations are provided for each type of APR.