The document discusses digestion and absorption in the gastrointestinal tract. It covers:
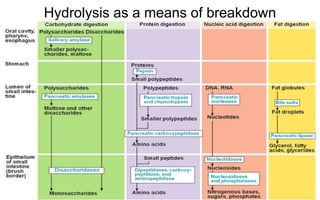
- The breakdown of large food molecules into smaller molecules that can be absorbed (monomers) through hydrolysis by enzymes.
- The four main food substances (carbohydrates, proteins, lipids, nucleic acids) and how each is broken down.
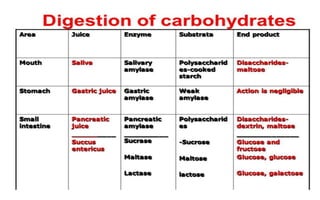
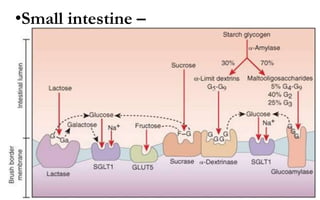
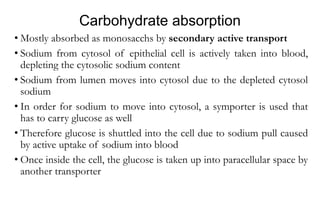
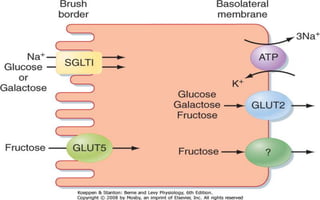
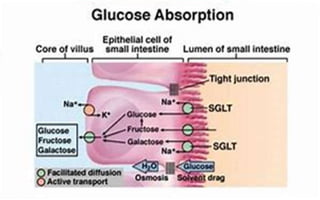
- Carbohydrates are broken down by enzymes in the mouth, stomach, and small intestine into monosaccharides that are then absorbed.
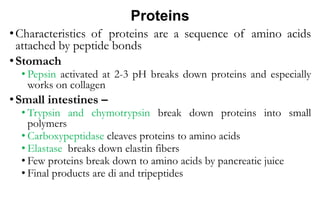
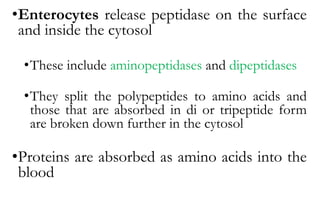
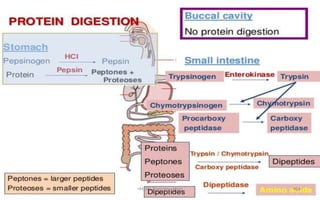
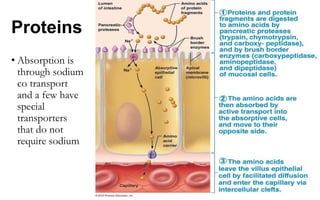
- Proteins are broken down by enzymes in the stomach and small intestine into dipeptides, tripeptides, and amino acids that are then absorbed.
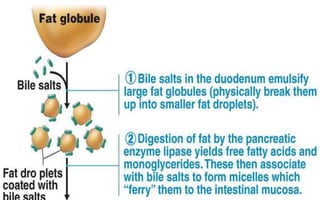
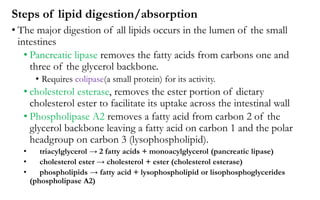
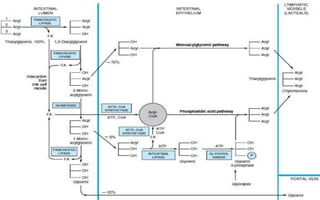
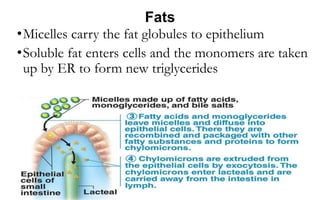
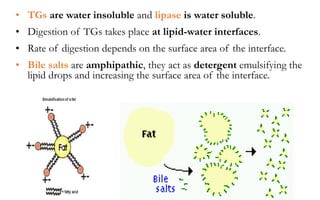
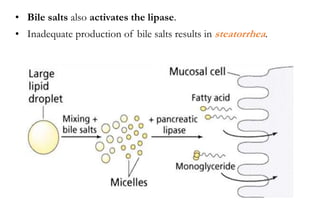
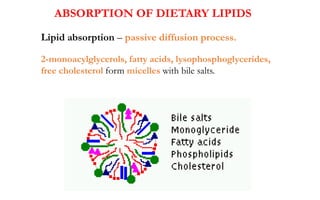
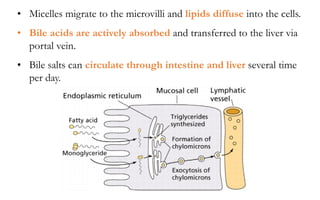
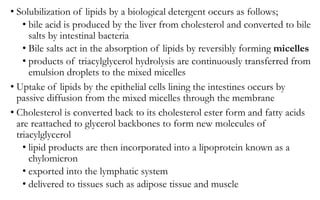
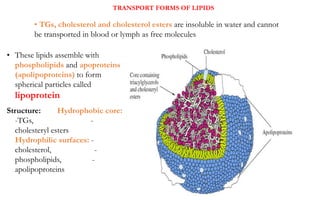
- Lipids are emulsified by bile salts for enzyme access and broken down by