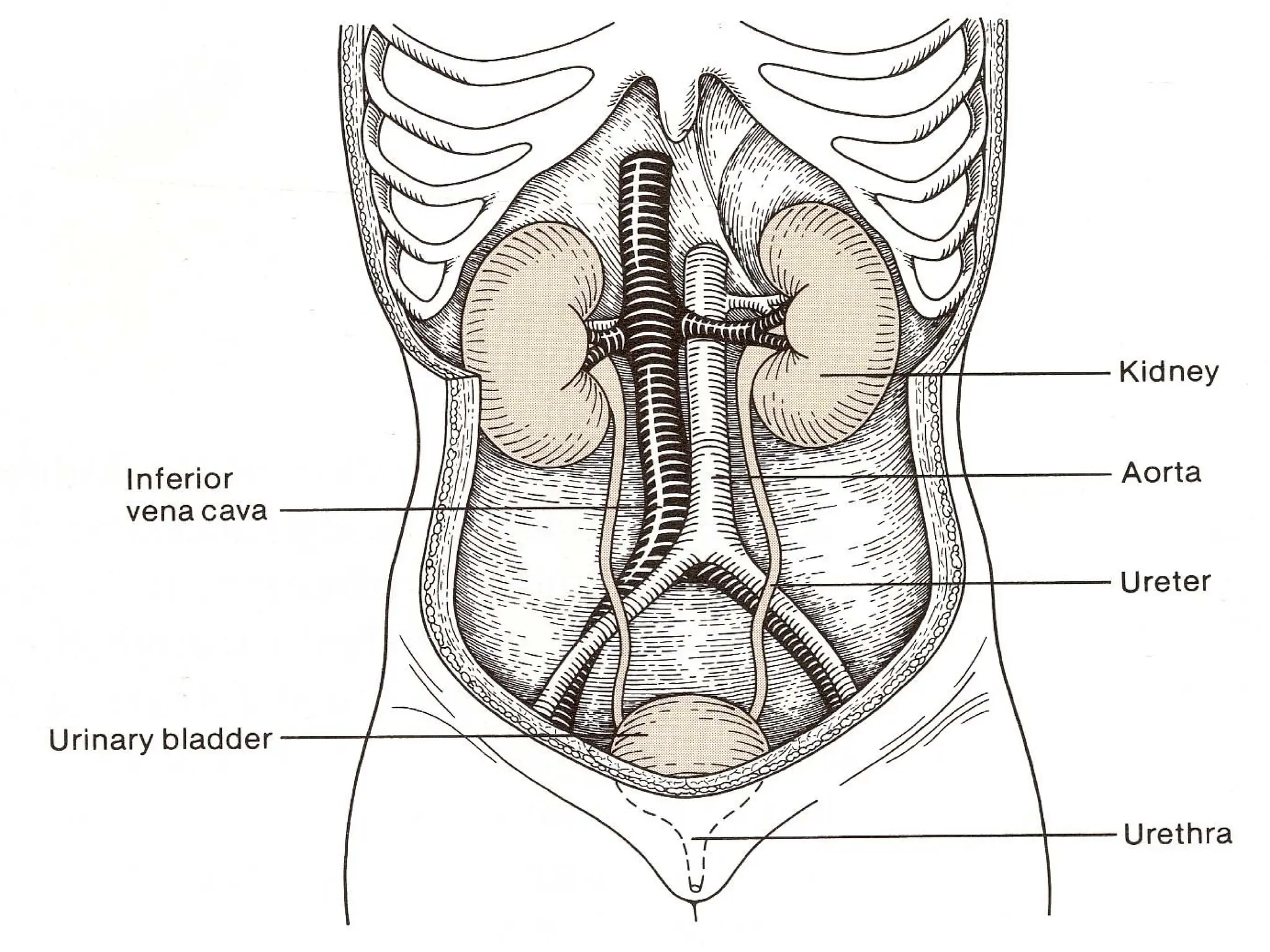
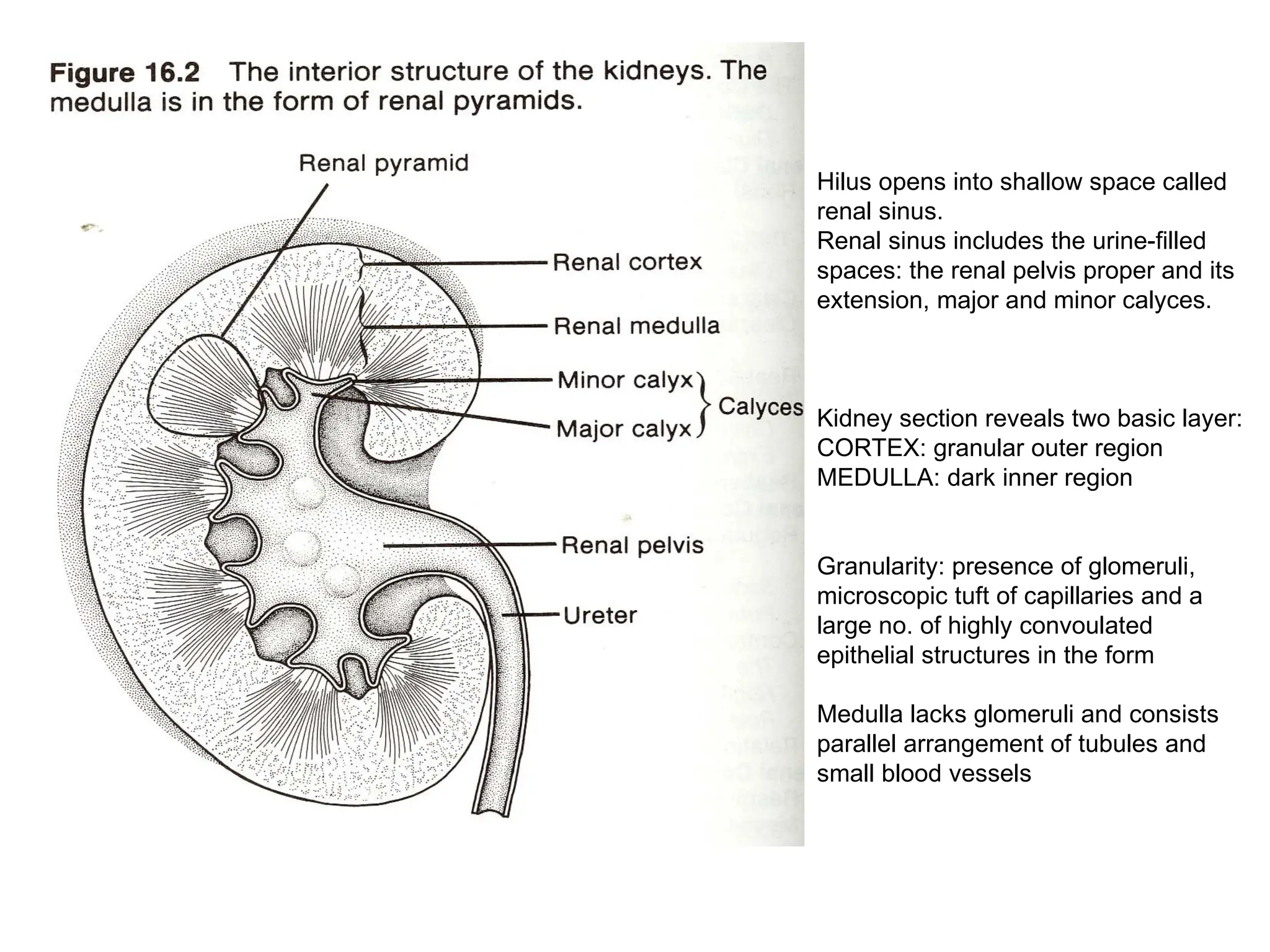
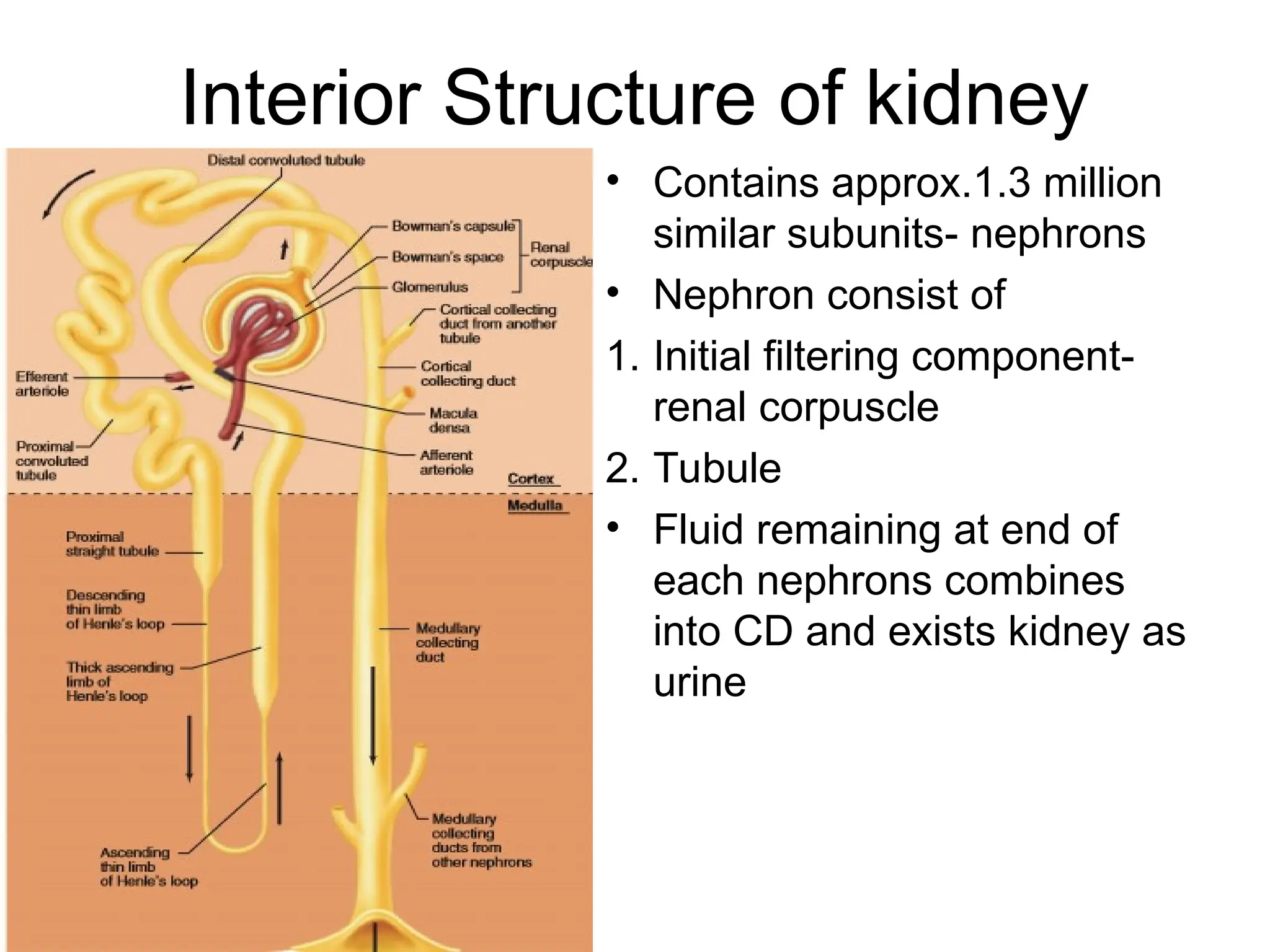
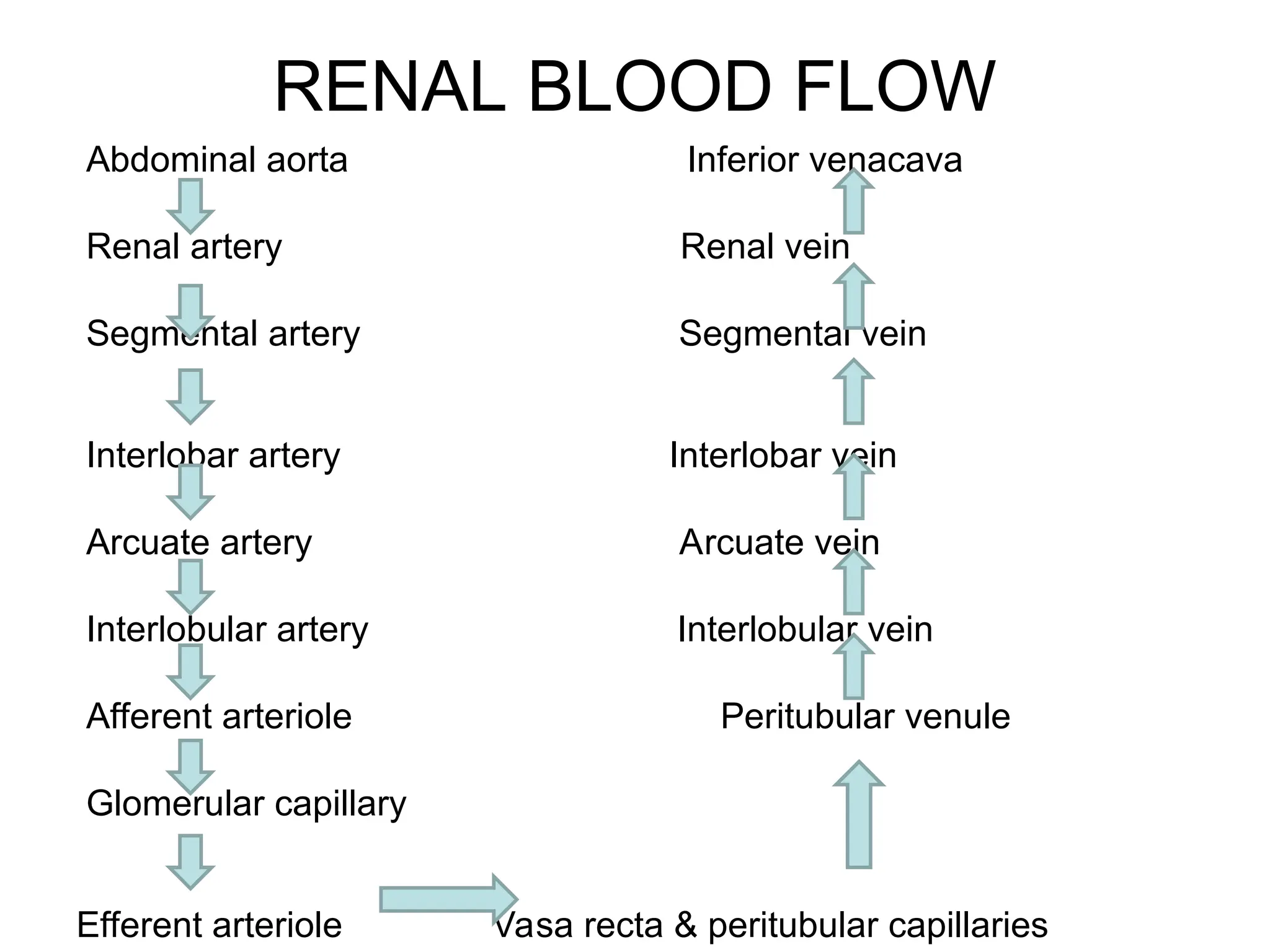
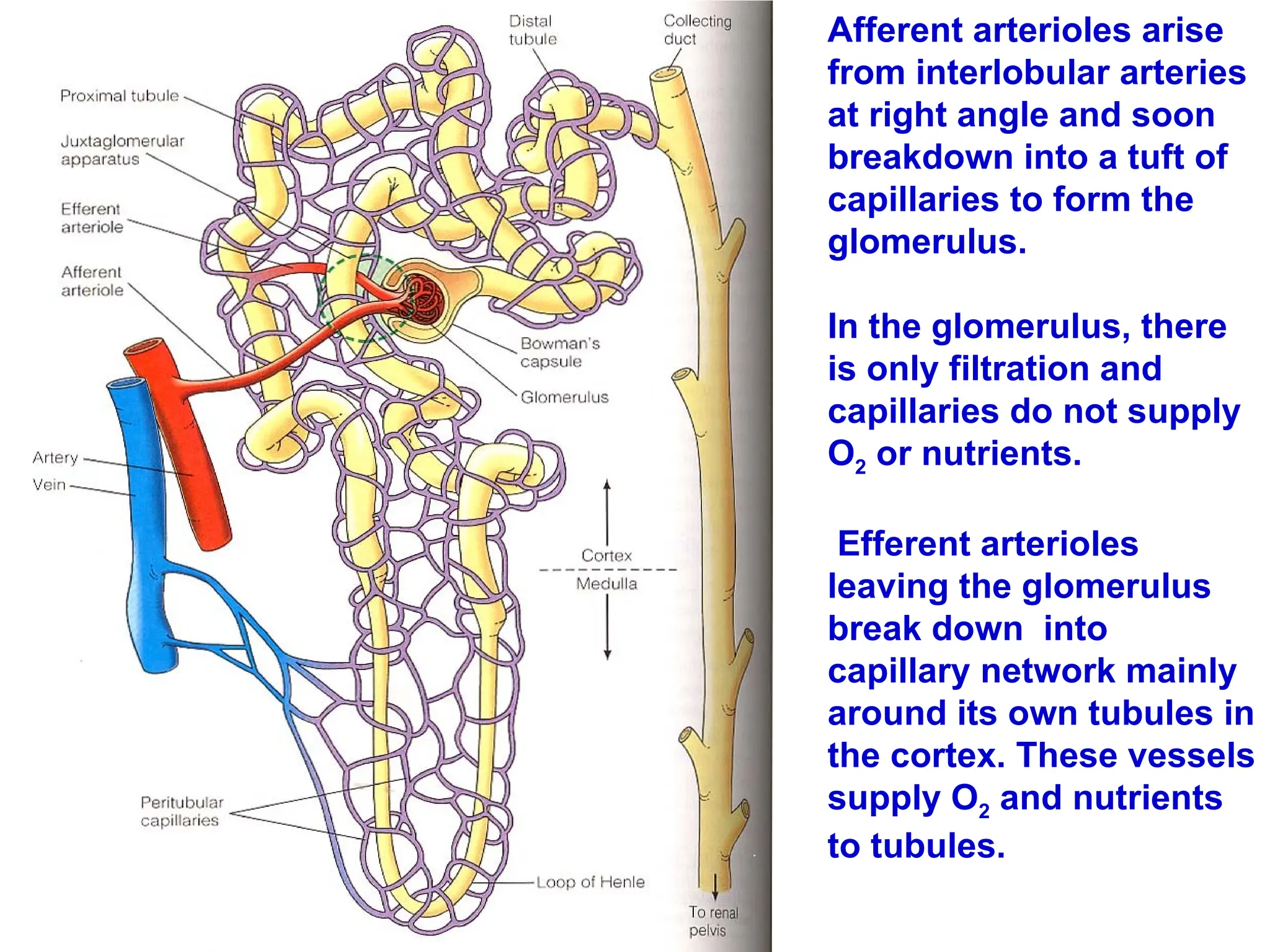
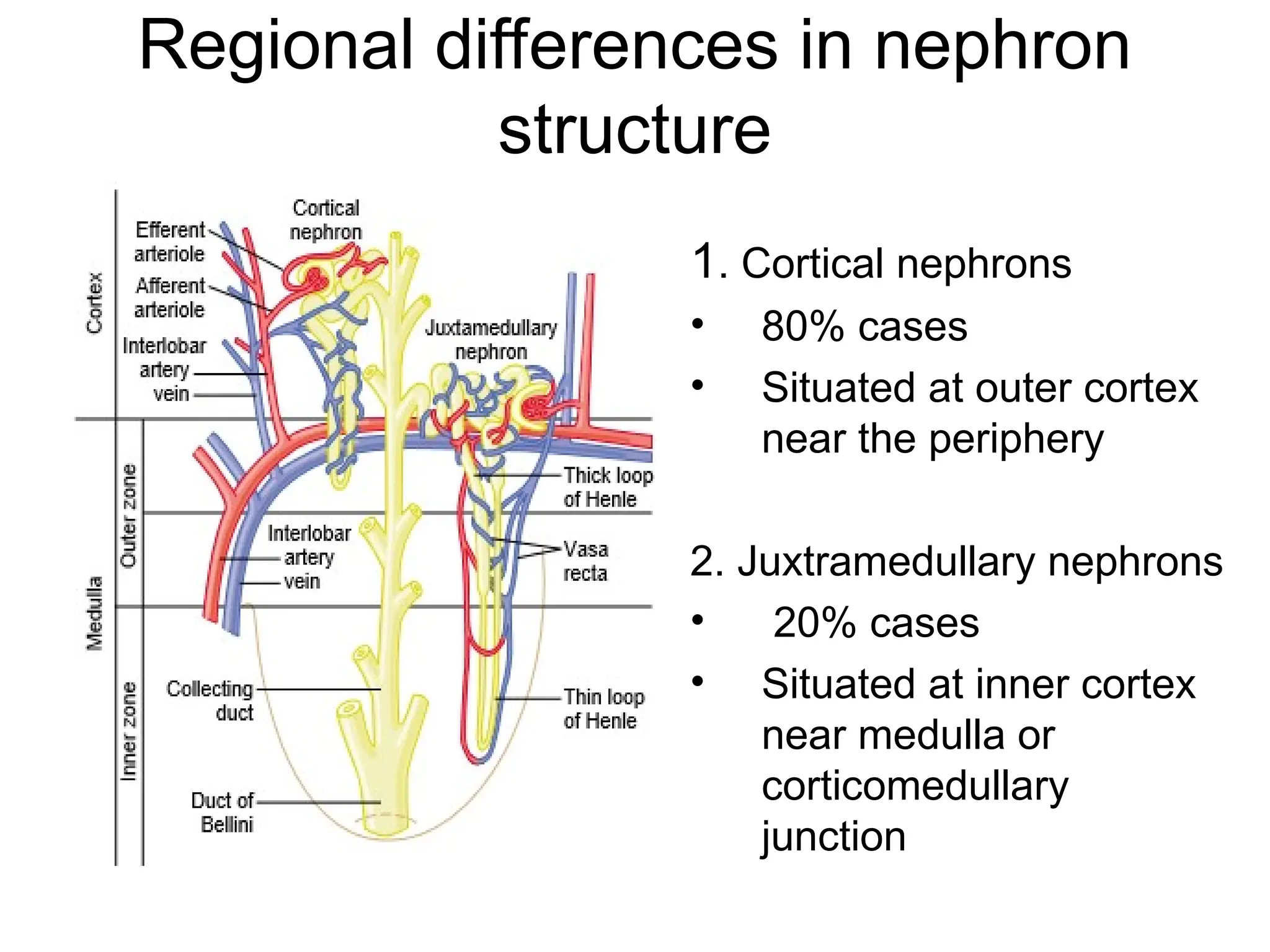
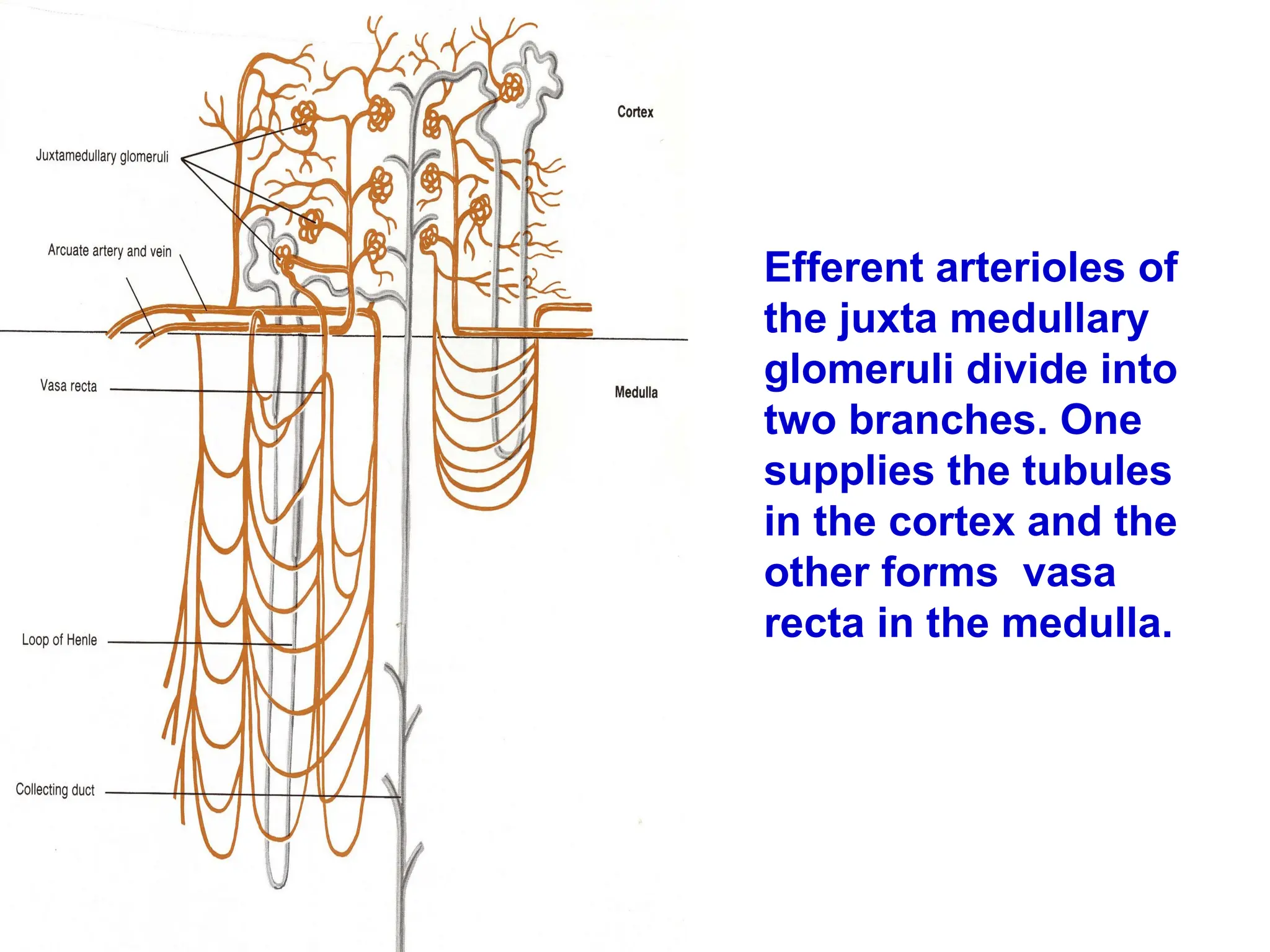
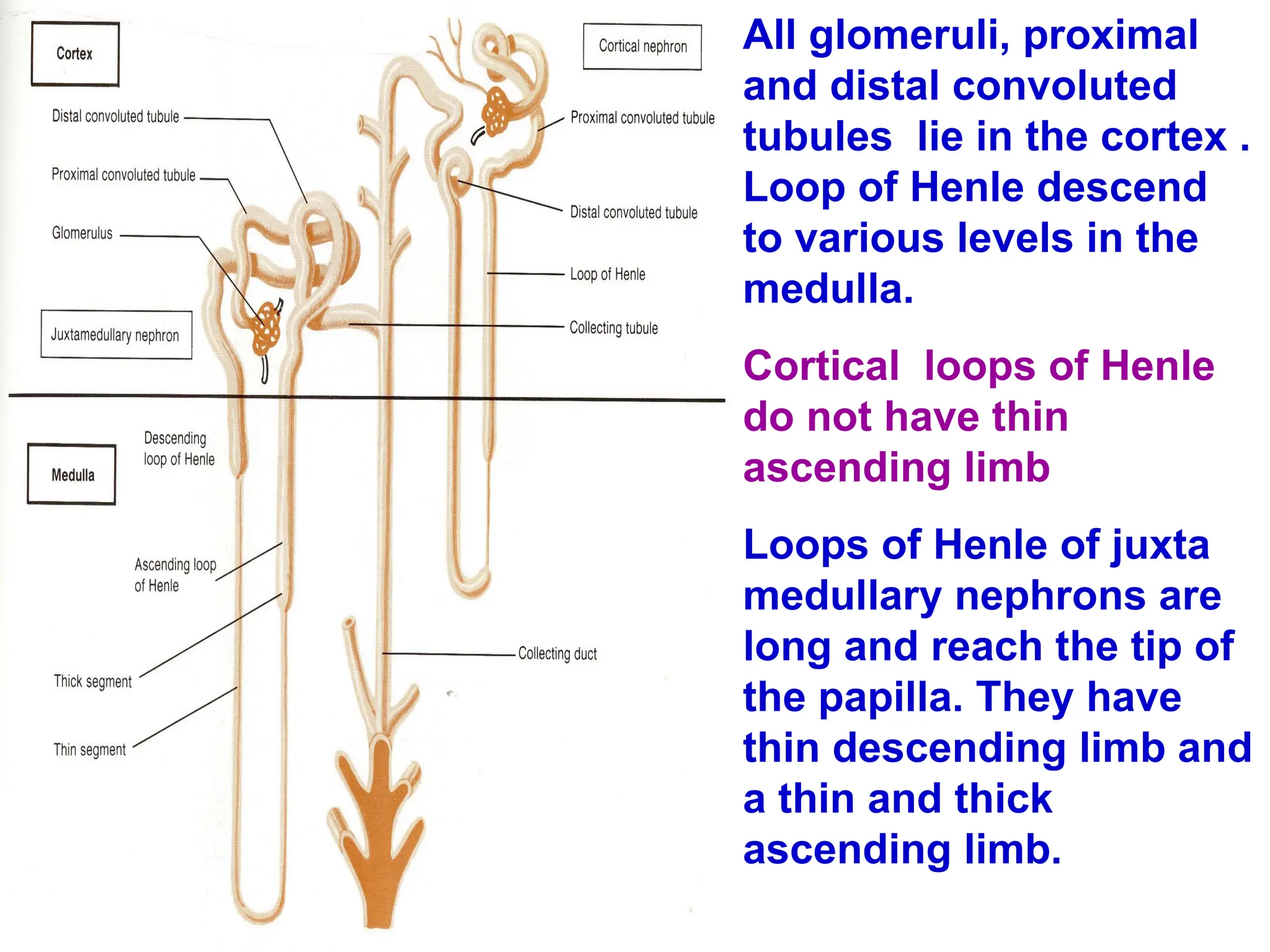
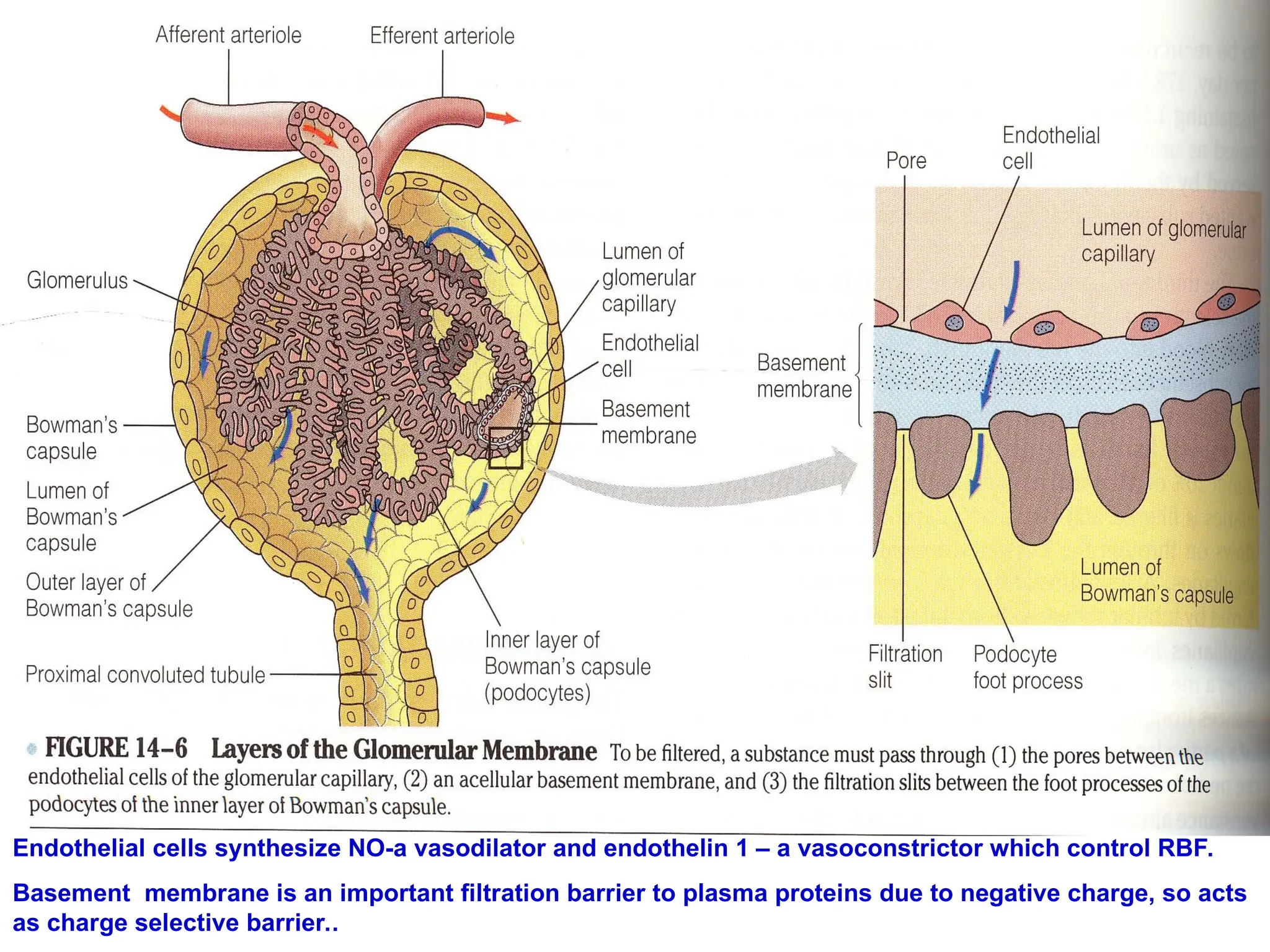
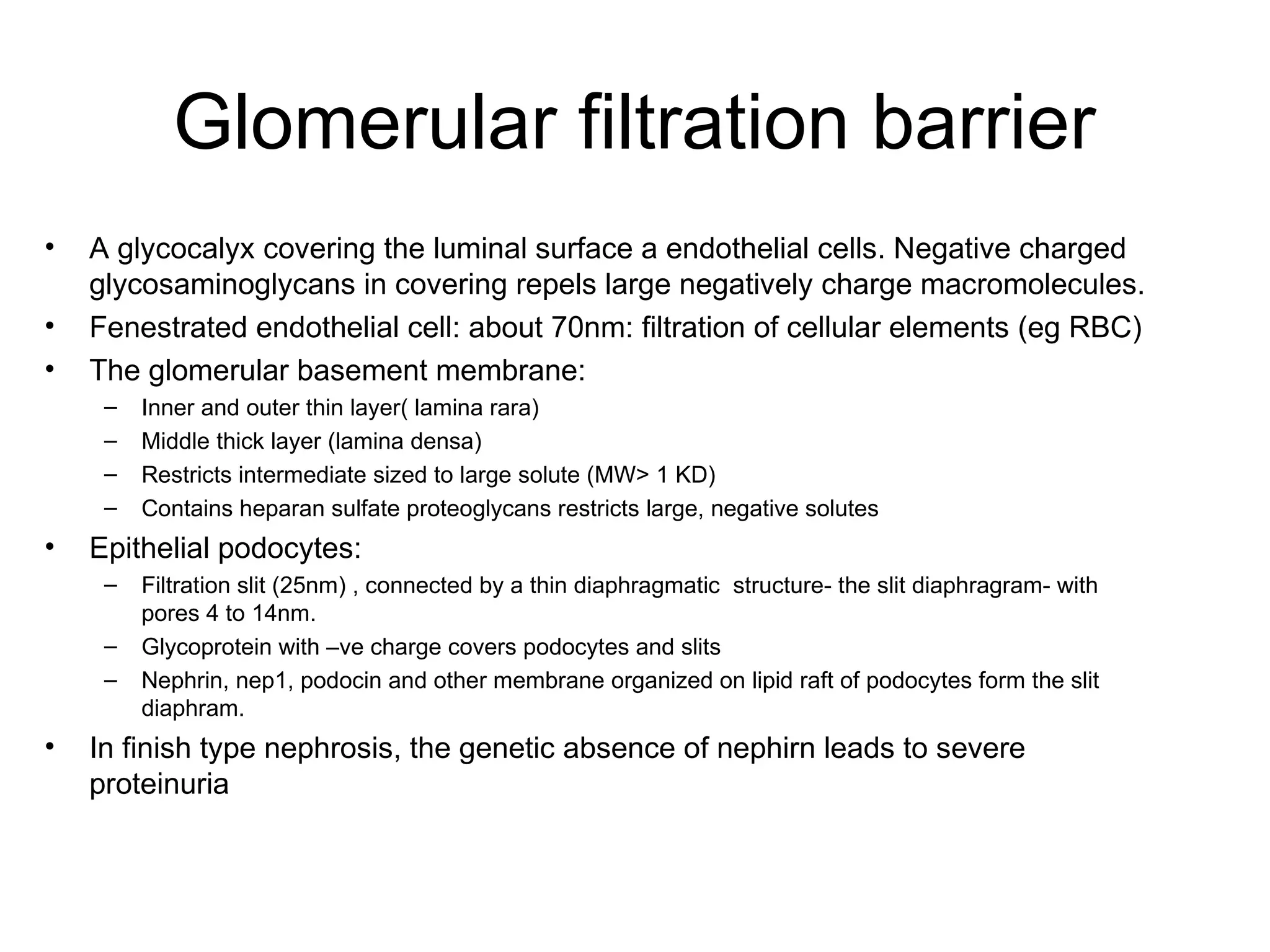
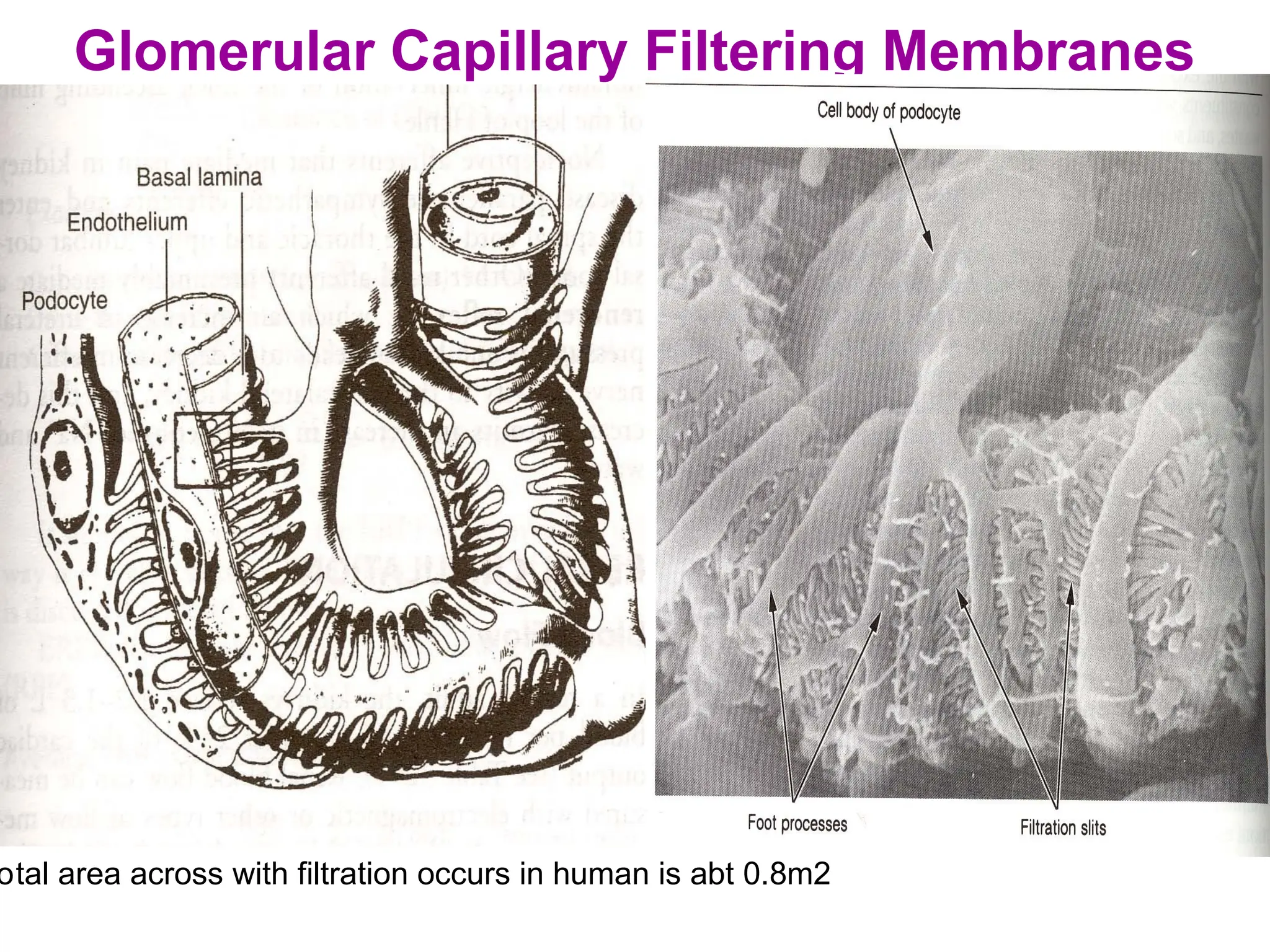
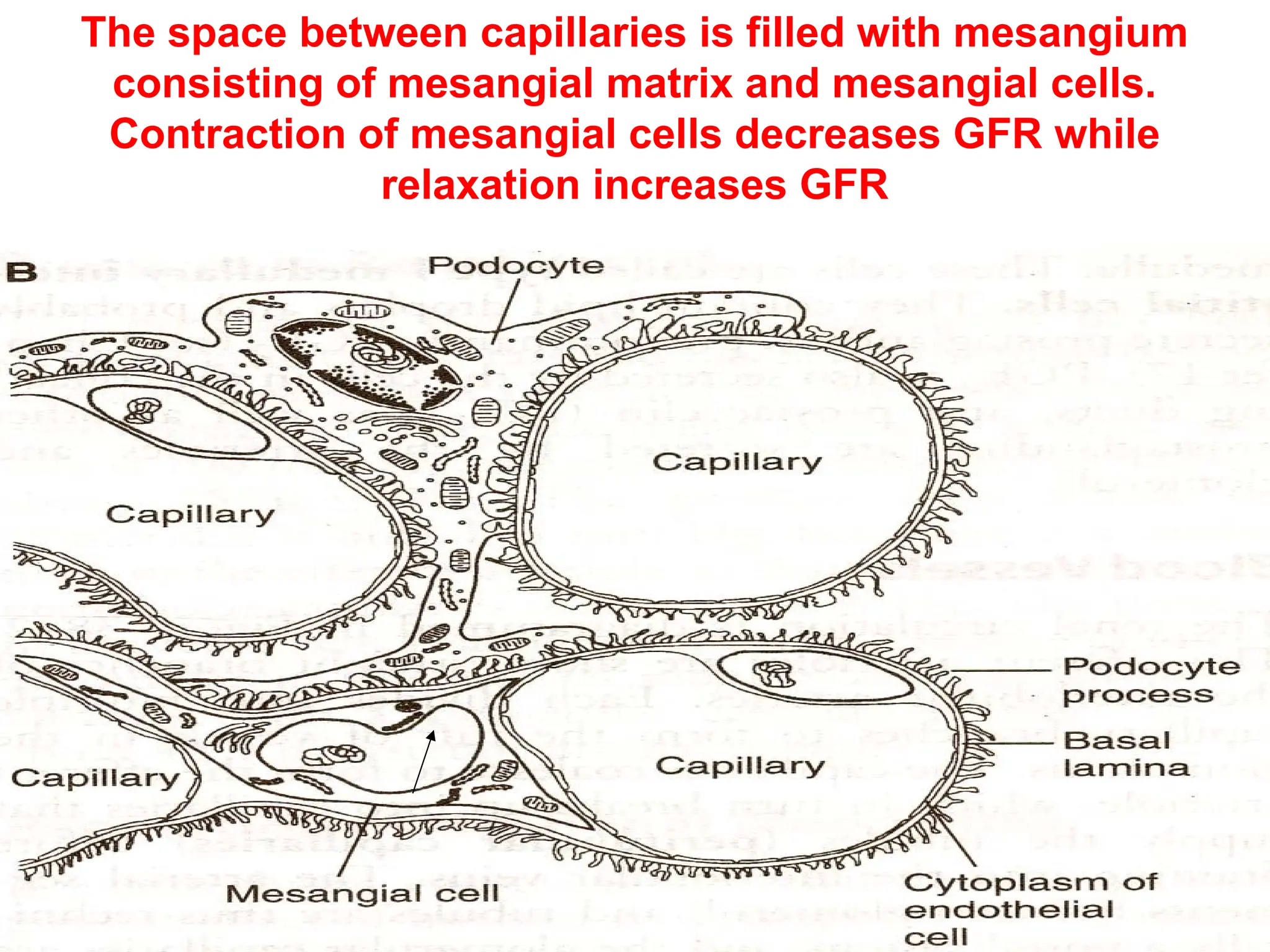
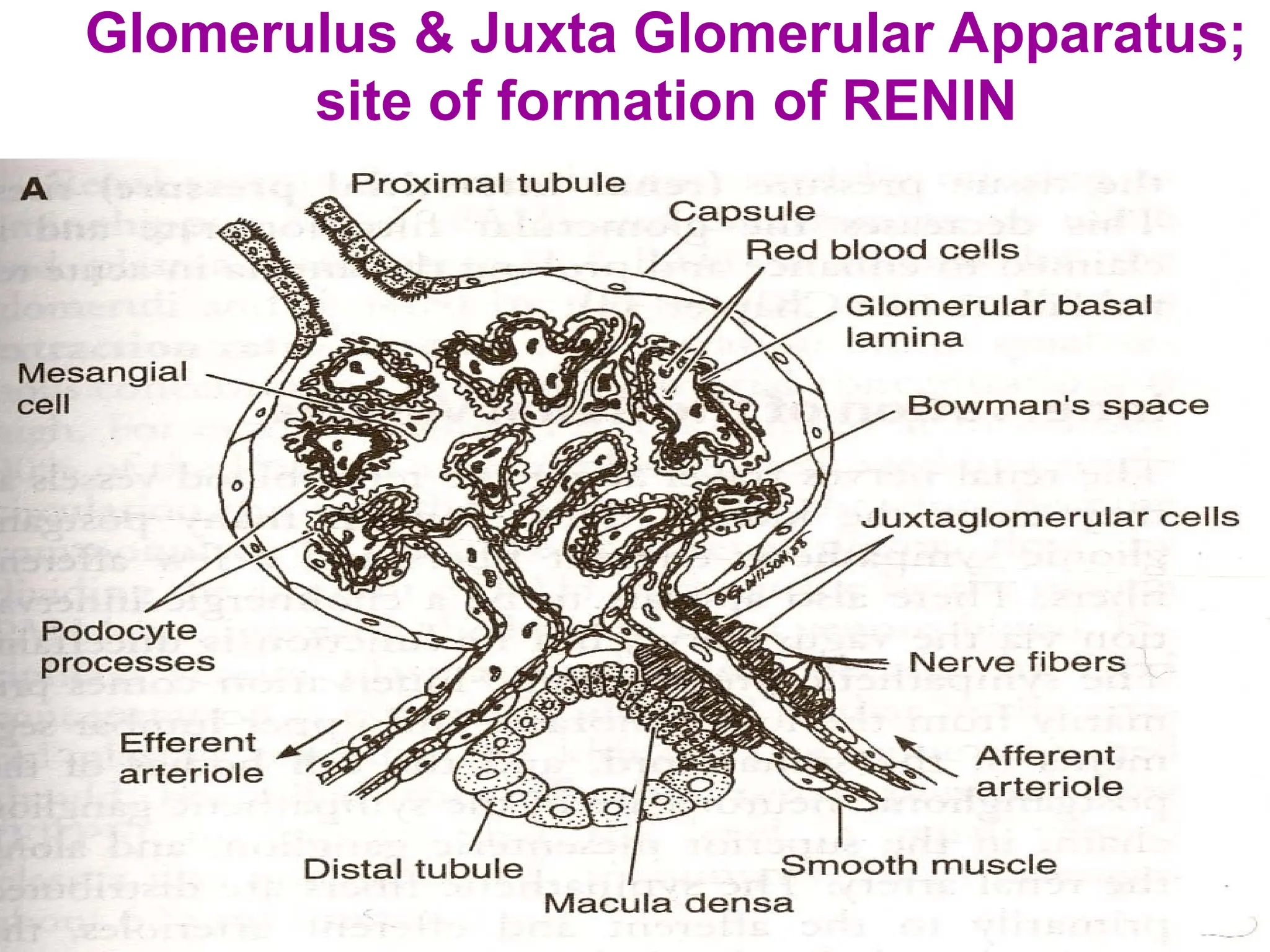
The document provides a detailed overview of the anatomy and function of the kidney, emphasizing the nephron as the functional unit responsible for regulating body fluid balance, blood pressure, electrolyte levels, and excreting waste. It describes the structure of the kidney, including its blood supply, nephron types, glomerular filtration, and the role of the juxtaglomerular apparatus in renin secretion. Auto-regulation of renal blood flow and the factors affecting it, including hormonal influences, are also discussed.