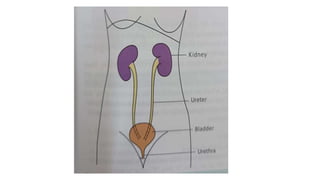
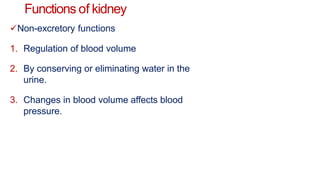
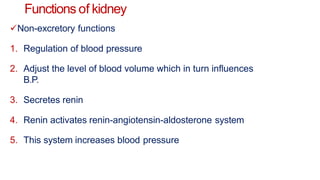
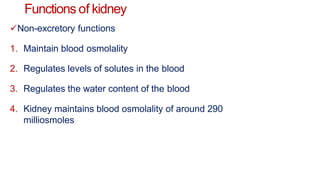
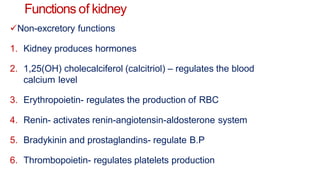
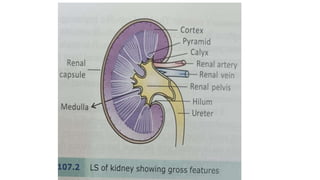
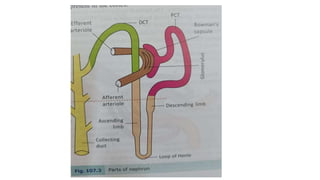
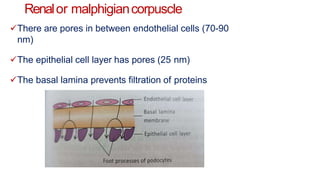
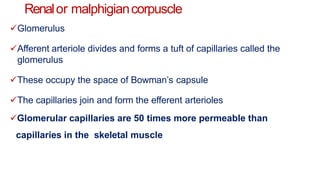
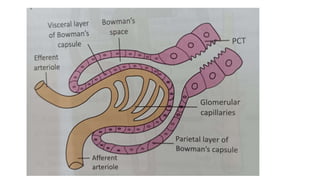
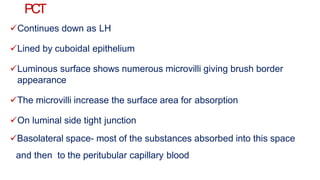
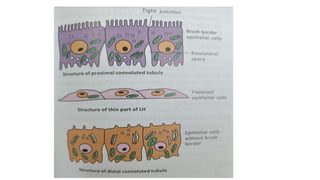
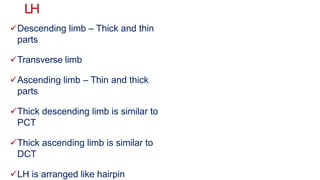
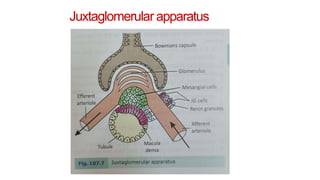
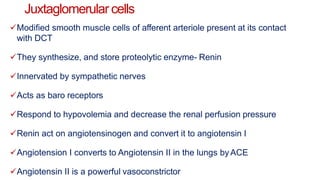
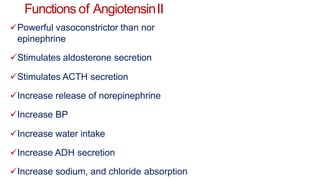
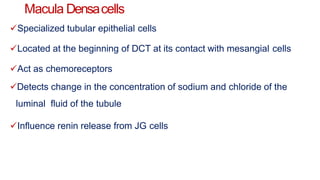
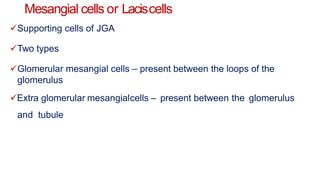
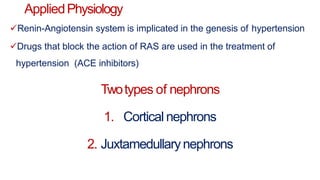
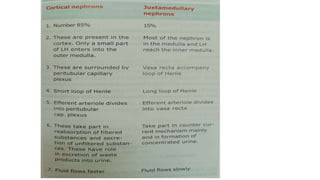
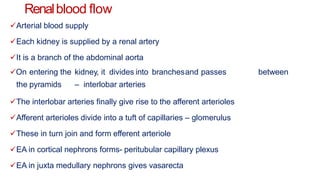
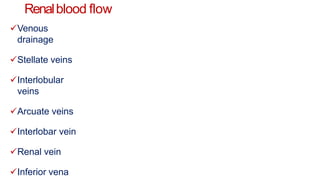
The document describes the structure and function of the kidney and renal circulation. It discusses the key components and functions of the nephron including the glomerulus, proximal convoluted tubule, loop of Henle, distal convoluted tubule and collecting duct. It also describes the juxtaglomerular apparatus and its role in regulating blood pressure via the renin-angiotensin system. Additionally, it outlines the special features of renal circulation including its high pressure, permeability and blood flow.