This document discusses several types of pneumonia including nosocomial, aspiration, and lung abscess pneumonia. It provides details on causative organisms, pathophysiology, clinical features, diagnosis and treatment. Key points include:
- Nosocomial pneumonia is associated with immunosuppression, antibiotics, and respirators. Common organisms are E. coli, Pseudomonas aeruginosa, and S. aureus.
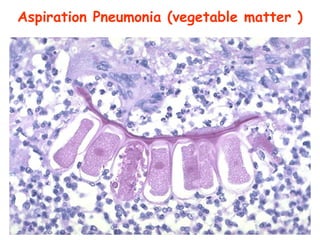
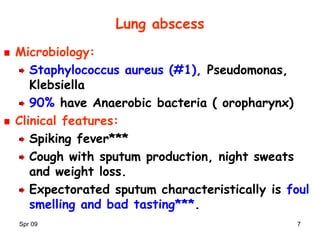
- Aspiration pneumonia results from gastric content aspiration and is characterized by necrotizing inflammation. Causative organisms include a mixture of oral aerobes and anaerobes like Bacteroides and S. pneumoniae.
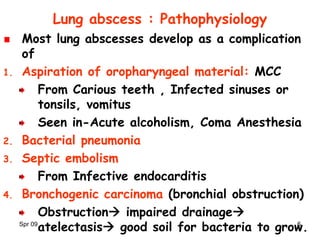
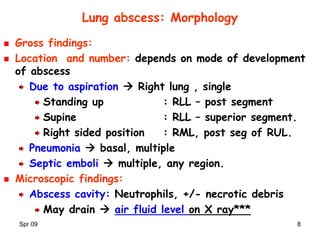
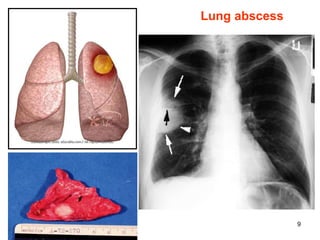
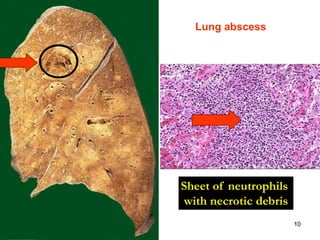
- Lung abscesses develop most commonly from aspiration or