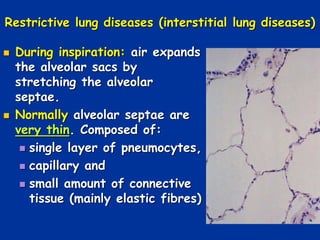
Restrictive lung diseases, particularly interstitial lung diseases (ILDs), are characterized by reduced lung compliance and increased lung elasticity, making it more difficult to breathe. The document outlines various types of ILDs, their causes, and pathophysiology, as well as associated clinical findings such as dyspnea, respiratory failure, and specific pulmonary function test results. Key causes include occupational exposures, such as pneumoconiosis from inhaling mineral dust, and conditions like sarcoidosis and idiopathic pulmonary fibrosis.