Pneumonia is an inflammation of lung parenchyma characterized by exudate accumulation in alveolar spaces. It is classified clinically (community-acquired, hospital-acquired, aspiration, etc.), morphologically (lobar, bronchopneumonia, interstitial), and etiologically (bacterial, viral, fungal, etc.). Typical presentations often involve sudden onset of fever and cough, while atypical presentations may manifest as low-grade fever and dry cough without consolidation.












![Spr 09 17Fall 07 17
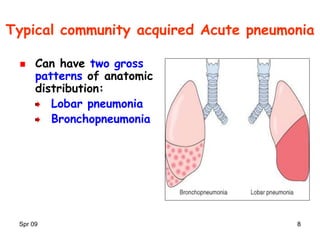
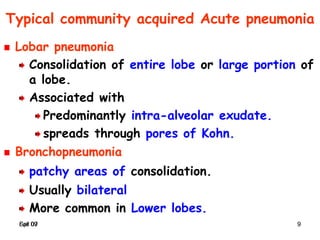
Typical community acquired pneumonia
Clinical findings
Sudden onset of
High fever
Cough productive of sputum [yellow-green (pus)
or rusty (bloody)].
Signs of consolidation in lungs on PE and X ray
Dullness to percussion
Increased vocal tactile fremitus
Chest X ray : first step in management***.
Radio-opaque lobe Lobar pneumonia
Focal opacities Bronchopneumonia](https://image.slidesharecdn.com/03respiratory-infection1-200403190748/85/03-Respiratory-infection1-17-320.jpg)