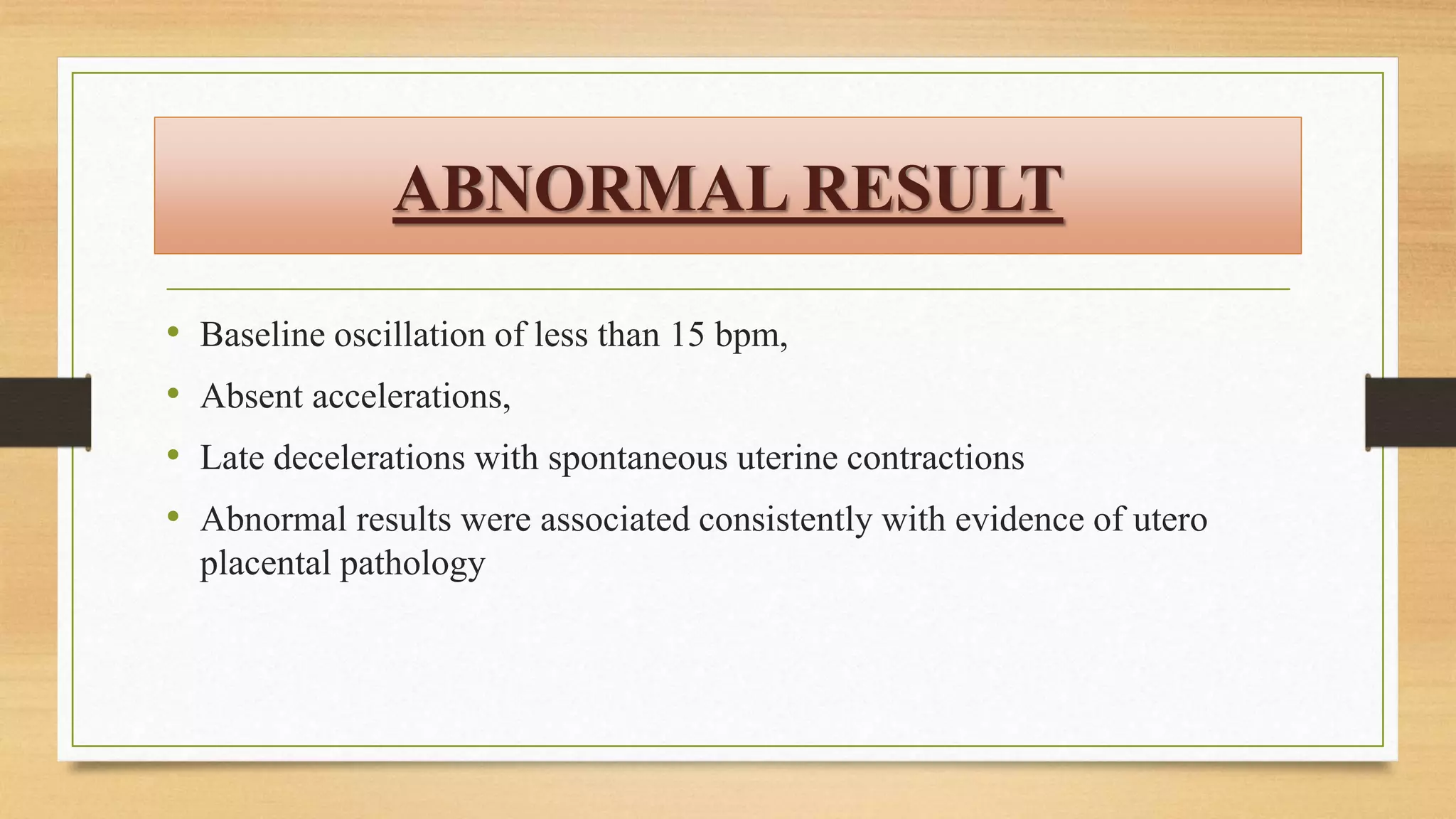
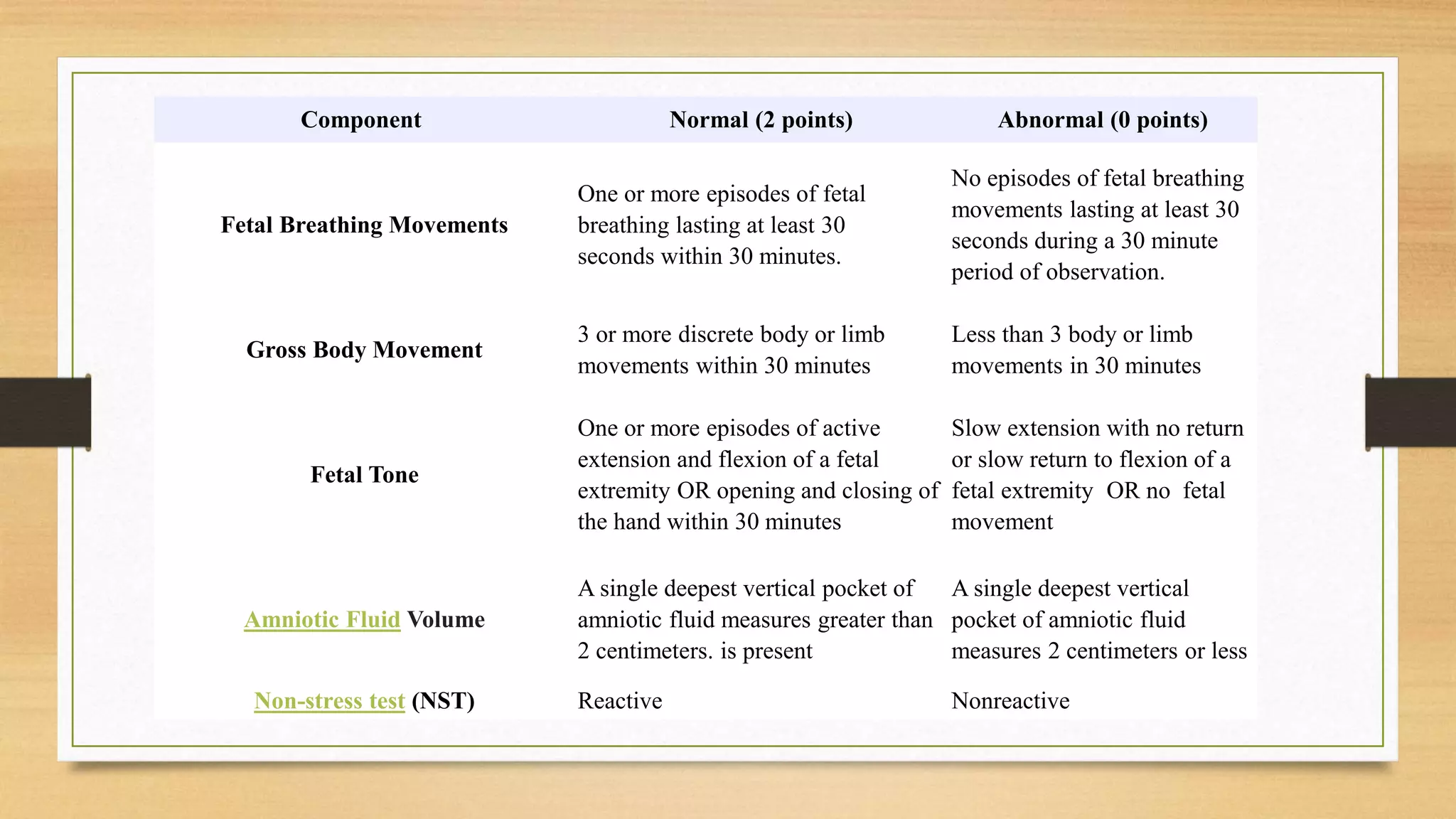
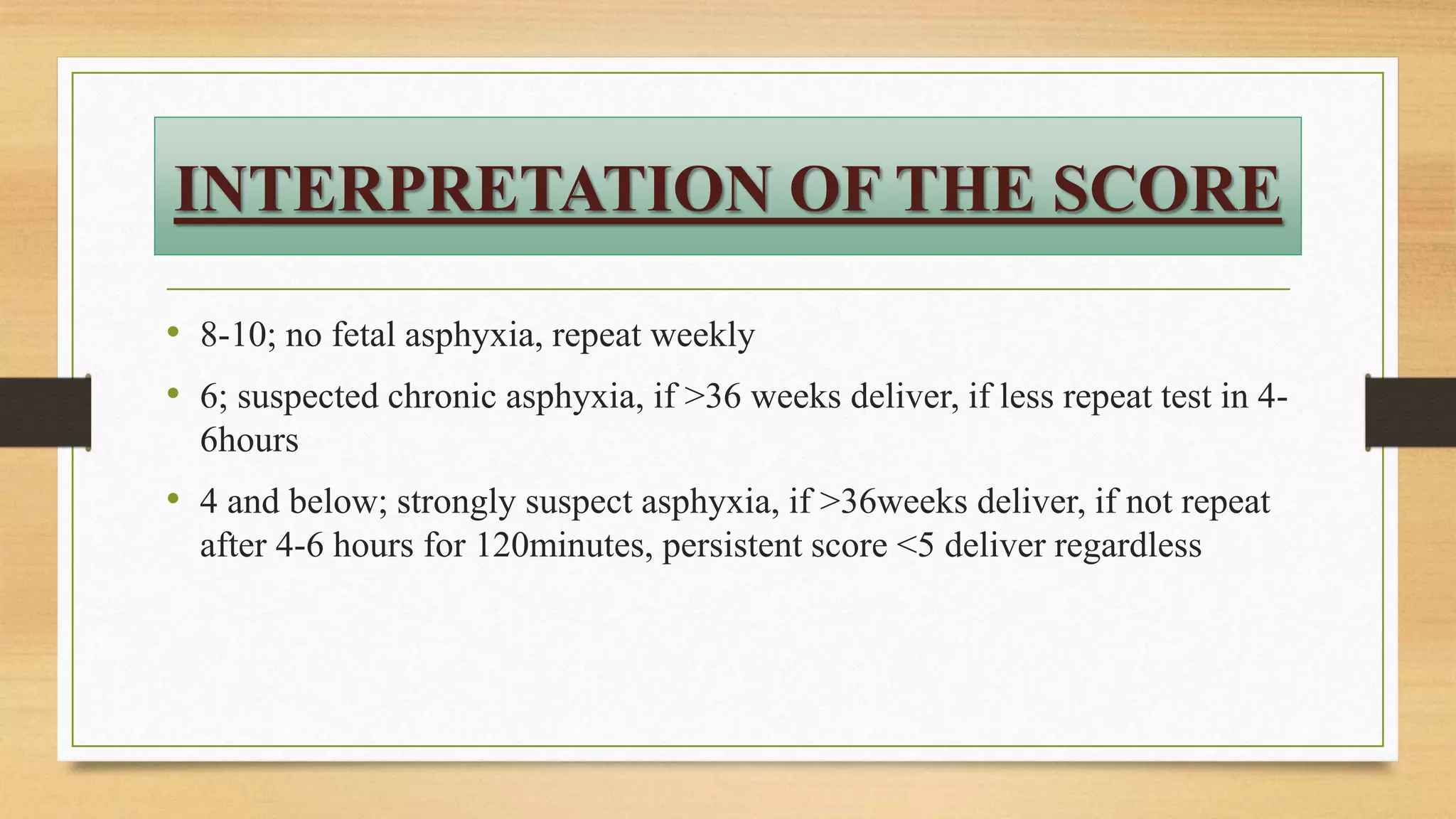
The document discusses the biophysical profile (BPP) as a technique for assessing fetal well-being, particularly in high-risk pregnancies, focusing on five key parameters: non-stress test (NST), fetal movements, fetal breathing, muscle tone, and amniotic fluid volume. It outlines the scoring systems for these parameters, defines normal and abnormal results, and emphasizes the importance of fetal activity and monitoring through ultrasound and cardiotocography. The conclusion highlights the balance in antepartum management of high-risk pregnancies and the role of fetal surveillance tests, particularly the NST, in ensuring fetal health.