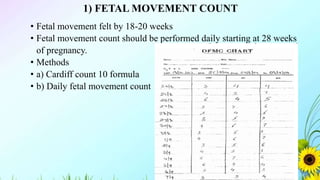
The biophysical profile is a non-invasive prenatal test designed to assess a fetus's well-being, typically conducted after 28 weeks of pregnancy. It combines fetal heart rate monitoring and ultrasound to evaluate heart rate, movements, muscle tone, and amniotic fluid levels, with the outcome providing valuable insights into potential complications in high-risk pregnancies. Various testing methods, including non-stress tests and cardiotocography, are utilized to ensure accurate assessments of fetal health.