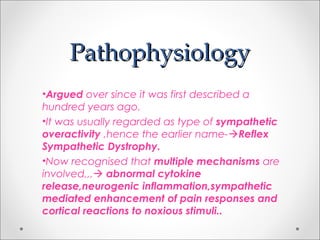
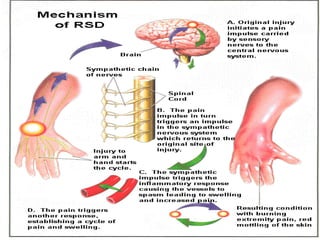
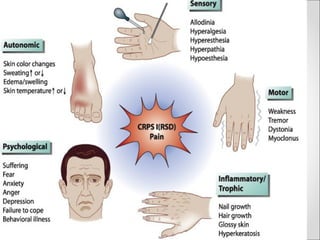
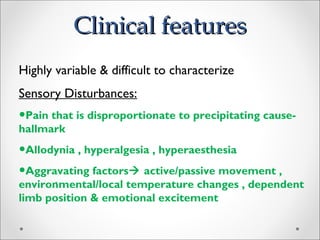
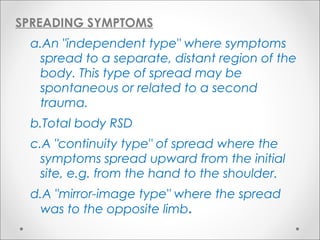
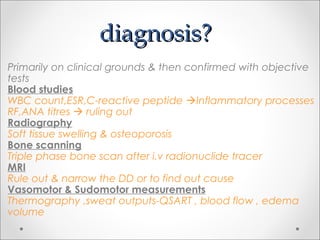
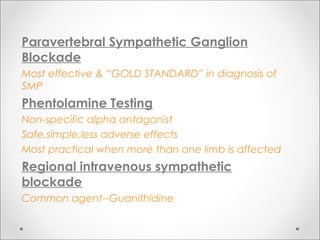
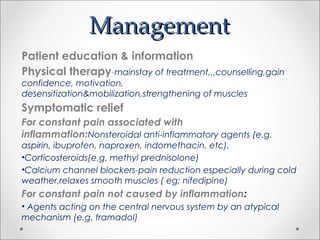
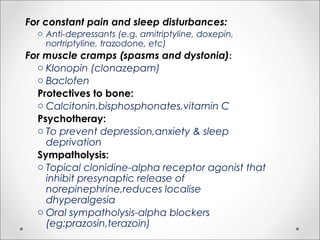
This document discusses complex regional pain syndrome (CRPS), formerly known as reflex sympathetic dystrophy. It defines CRPS as a multi-symptom syndrome that usually affects one or more extremities and is characterized by disproportionate pain, vasomotor instability, trophic skin changes, and regional osteoporosis. Trauma is a common precipitating factor. Management involves a multidisciplinary approach including physical therapy, medications to relieve symptoms, and in some cases surgical or injection-based treatments.