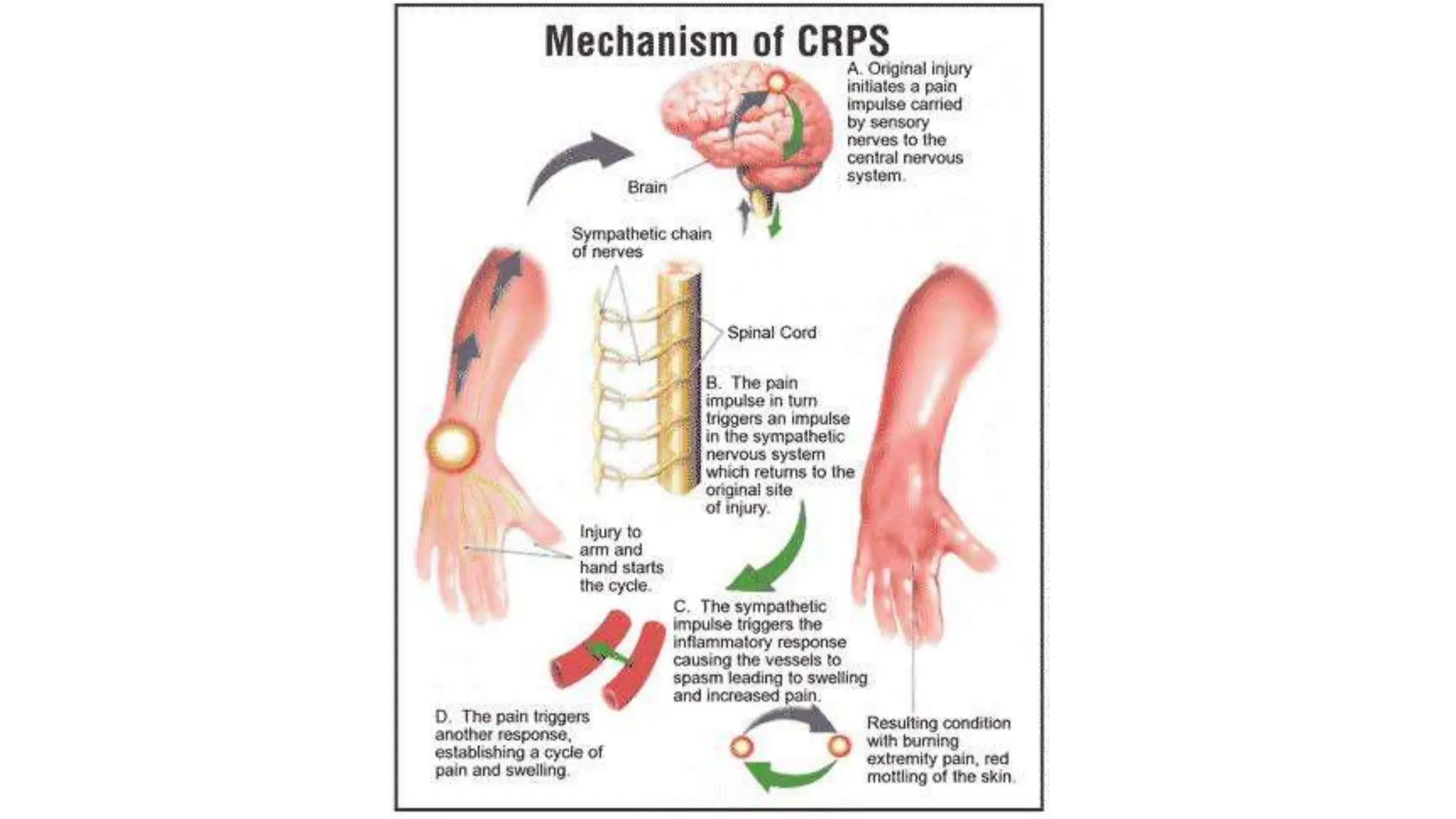
Complex regional pain syndrome (CRPS) is a pain disorder characterized by persistent regional pain that is disproportionate to a known injury, with varying degrees of type I and type II. The syndrome is characterized by autonomic and sensory dysfunction, and can affect individuals of all ages, with a higher prevalence in females. Treatment options include noninvasive therapies such as medication and physical therapy, with more invasive options available as necessary.






















![Examination
Autonomic Dysfunction:
The majority of patients with CRPS have bilateral differences in limb temperature and the skin
temperature depends of the chronicity of the disease.
In the acute stages, temperature increases are often concomitant with a white or reddish
colouration of the skin and swelling.
where the syndrome is chronic, the temperature will decrease and is associated with a bluish
tint to the skin and atrophy.
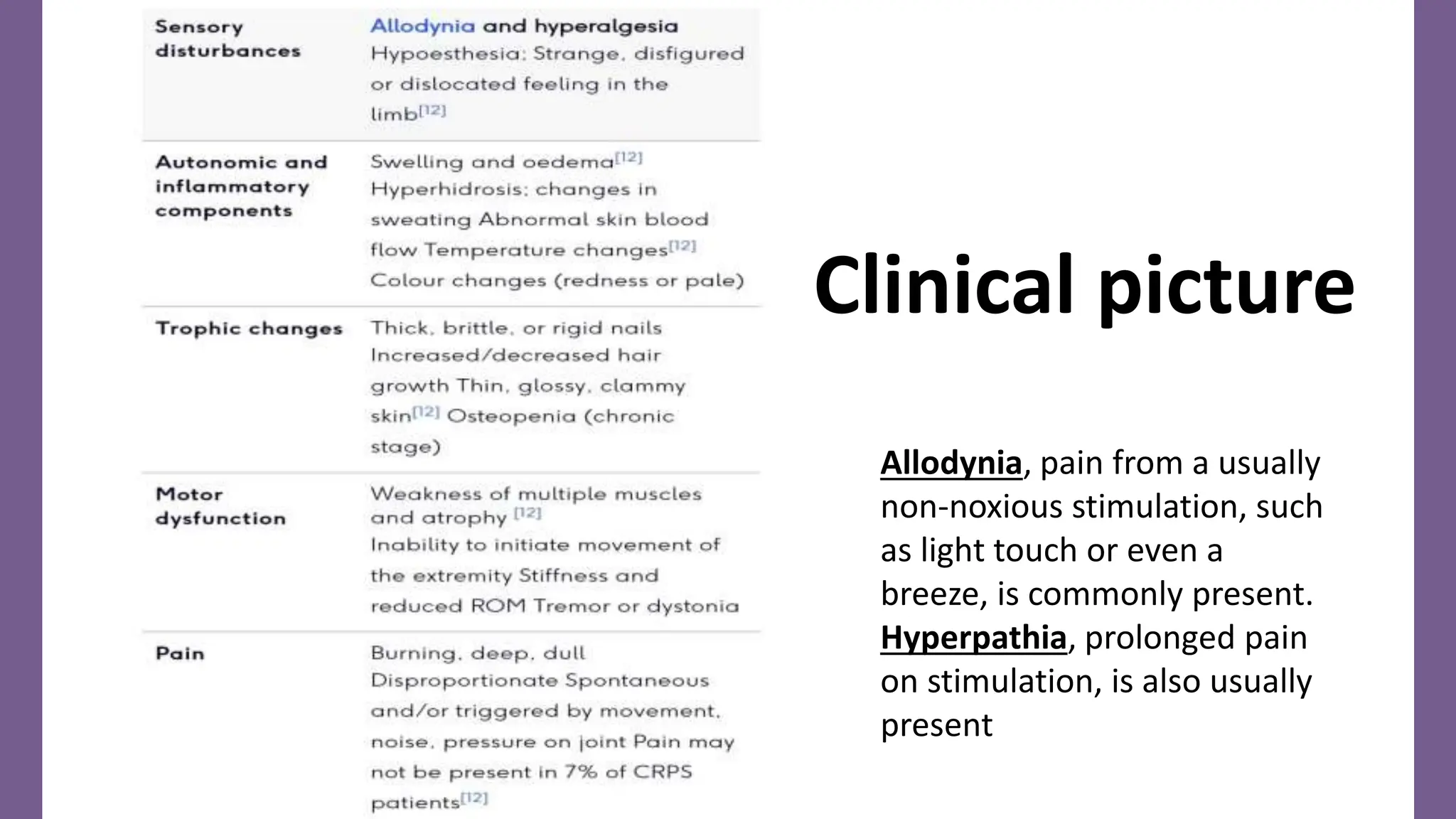
Motor Dysfunction:
Studies have shown that approximately 70% of the patients with CRPS show muscle weakness
in the affected limb, exaggerated tendon reflexes or tremor, irregular myoclonic jerks, and
dystonic muscle contractions. Muscle dysfunction often coincides with a loss of range of
motion in the distal joints.
Sensory Dysfunction:
The distal ends of the extremities require attention when examining a patient with CRPS.
However, common findings of regional neuropathic and motor dysfunction have shown us that
it is important to broaden the examination both proximally and contralaterally. [41]Light
touch, pinprick, temperature and vibration sensation should be assessed for a complete
picture of the CRPS.](https://image.slidesharecdn.com/crps-240625123034-83146fe0/75/All-about-Complex-Regional-Pain-Syndrome-pptx-28-2048.jpg)