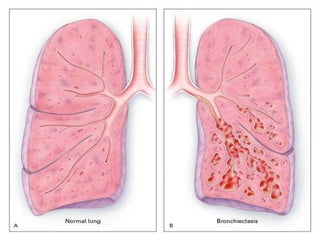
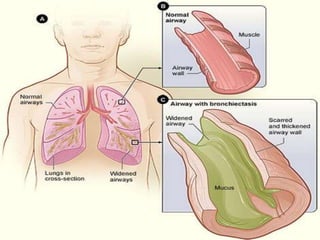
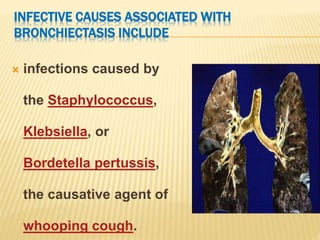
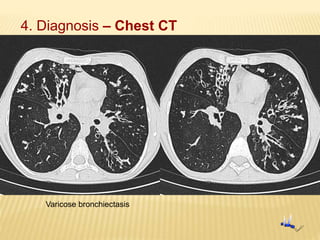
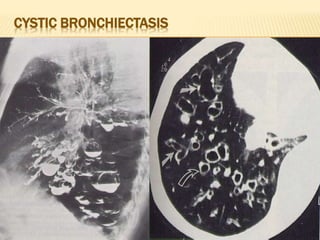
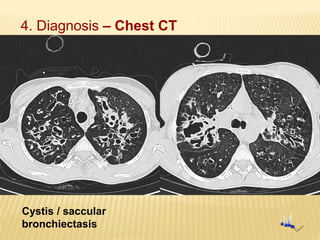
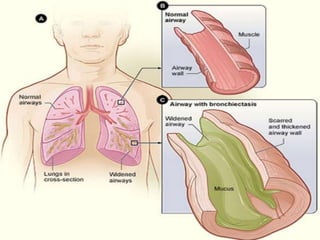
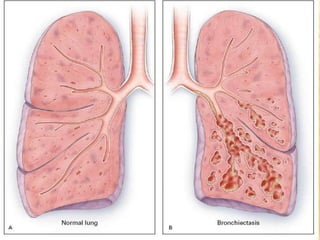
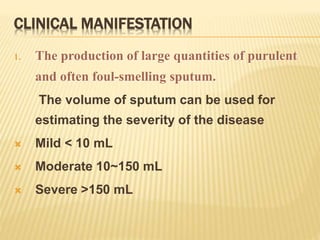
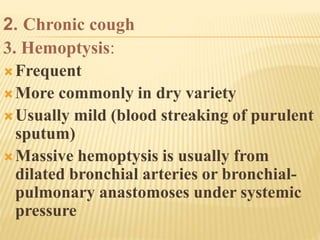
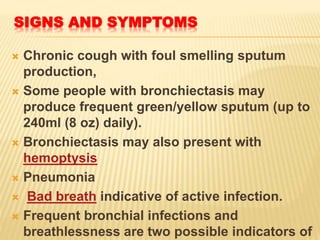
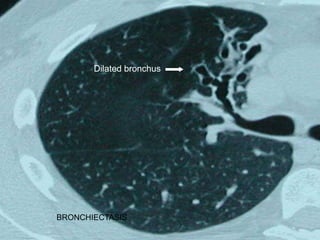
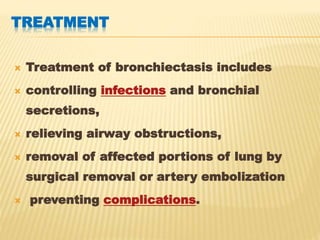
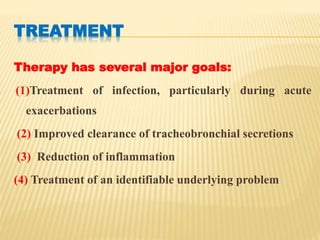
Bronchiectasis is a chronic lung condition defined by abnormal dilatation of the bronchi. It can be caused by infections, genetic conditions, or other lung diseases that damage the airways. People with bronchiectasis commonly produce large amounts of sputum and experience recurrent lung infections. Diagnosis is made through chest imaging like CT scans. Treatment focuses on airway clearance and controlling infections with antibiotics. Surgical options are available for severe cases involving hemorrhage or localized disease.