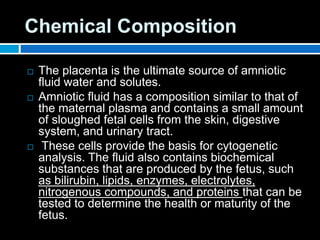
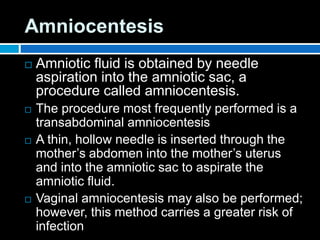
Amniotic fluid provides protection and nutrients for the developing fetus. It is regulated by a balance of fetal production and absorption. Amniocentesis extracts amniotic fluid for analysis of fetal health, maturity, and genetic abnormalities. Tests of amniotic fluid assess lung maturity through measurements of surfactant components like lecithin and phosphatidylglycerol that prevent lung collapse.