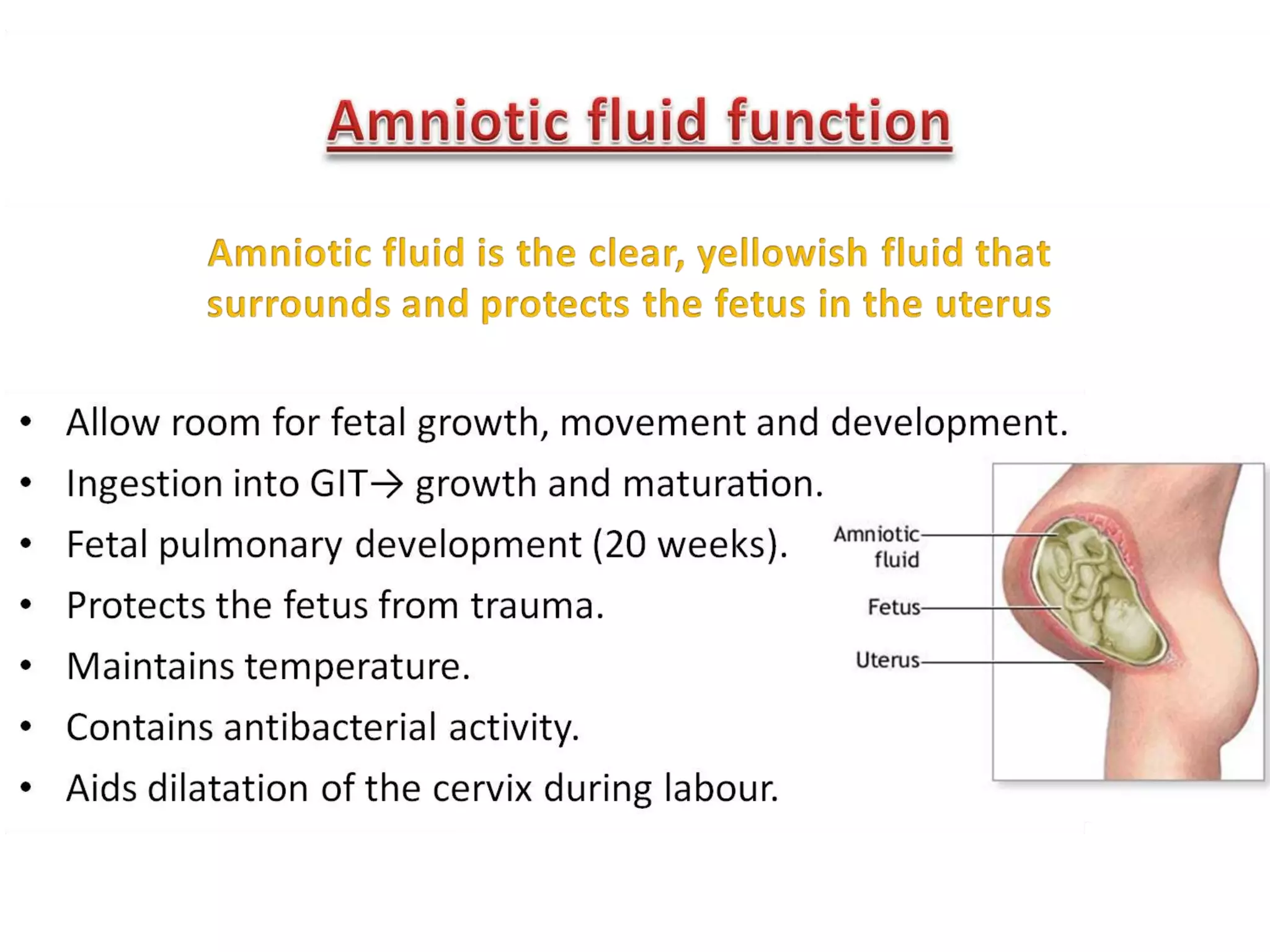
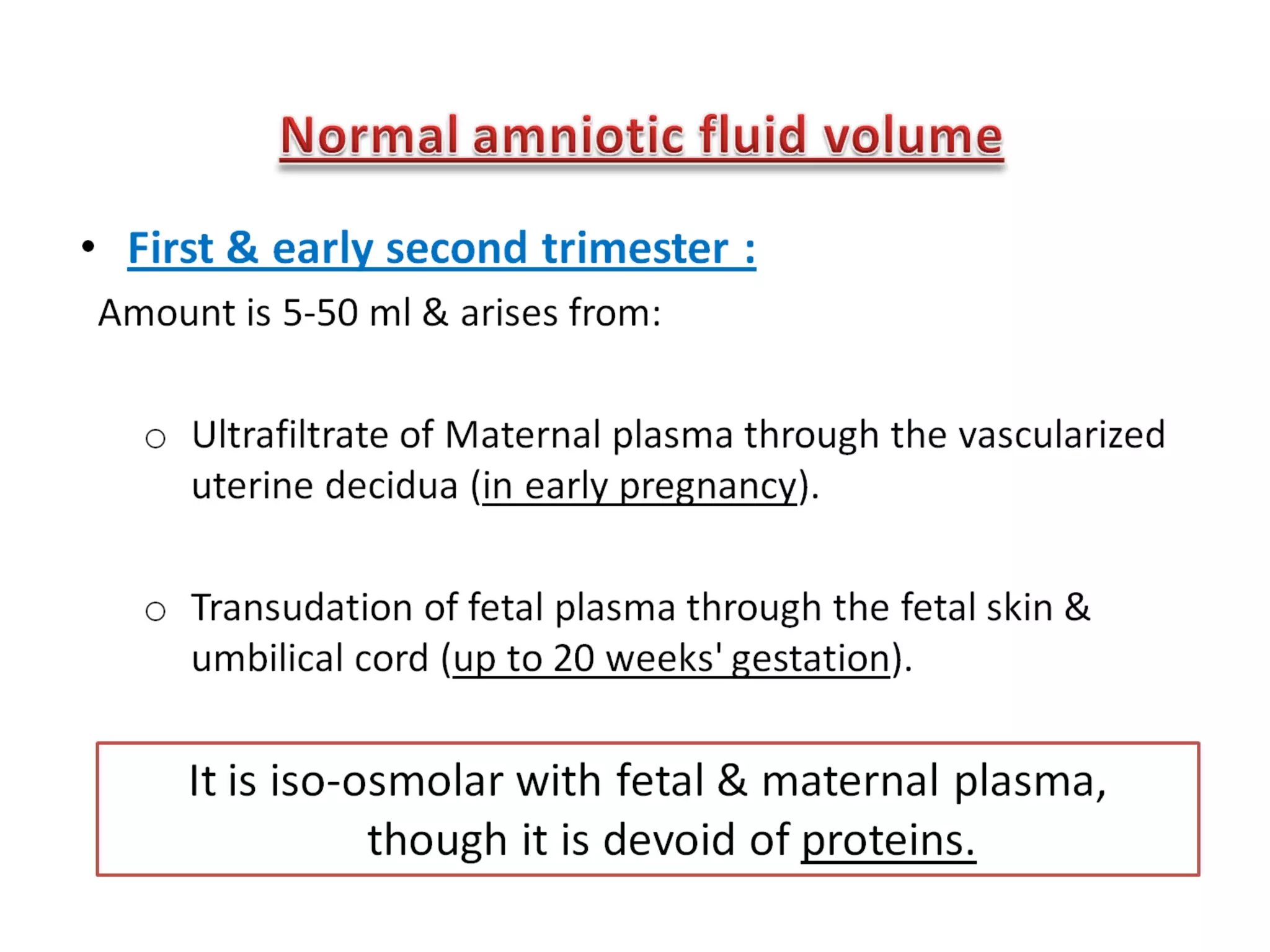
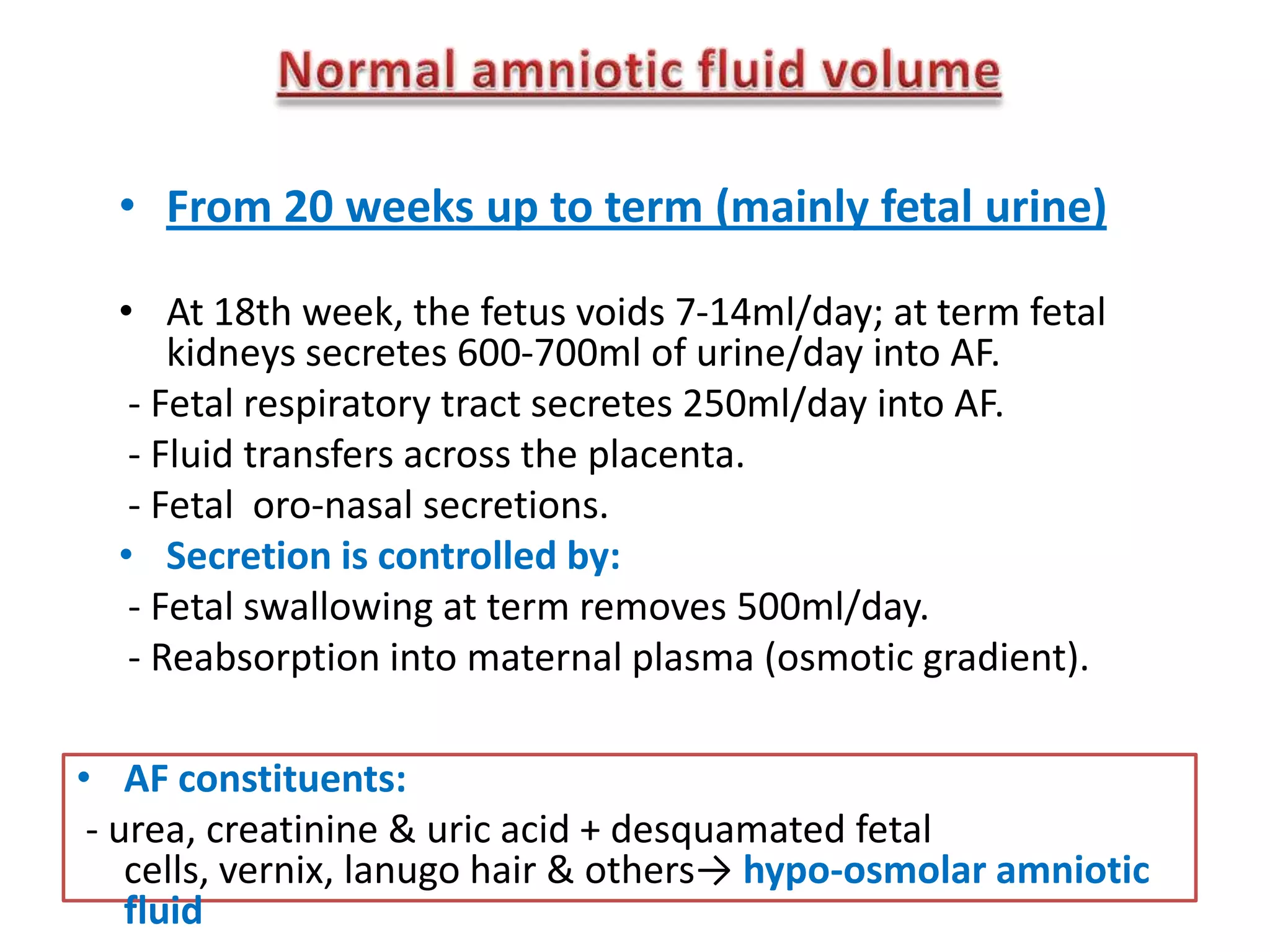
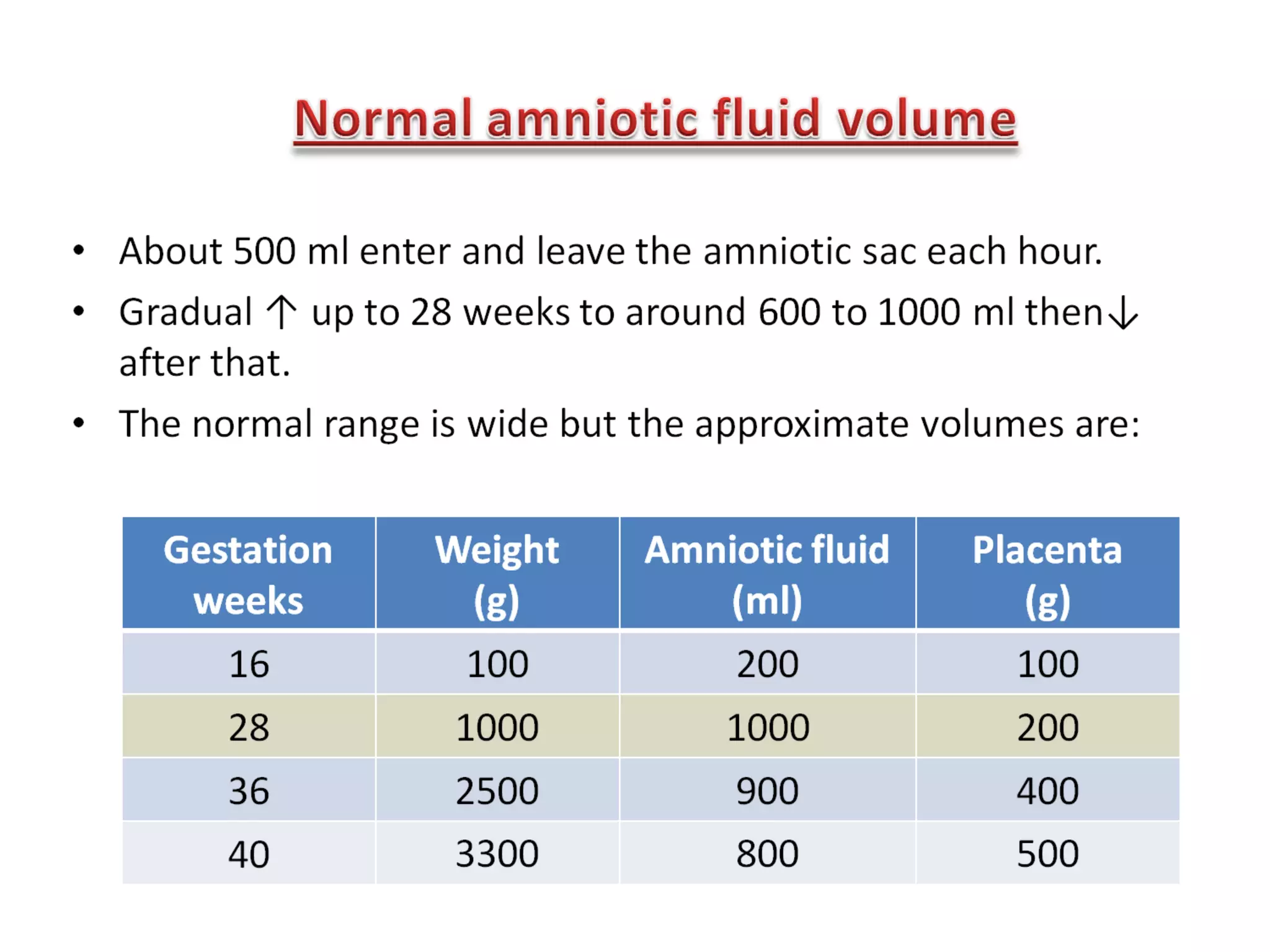
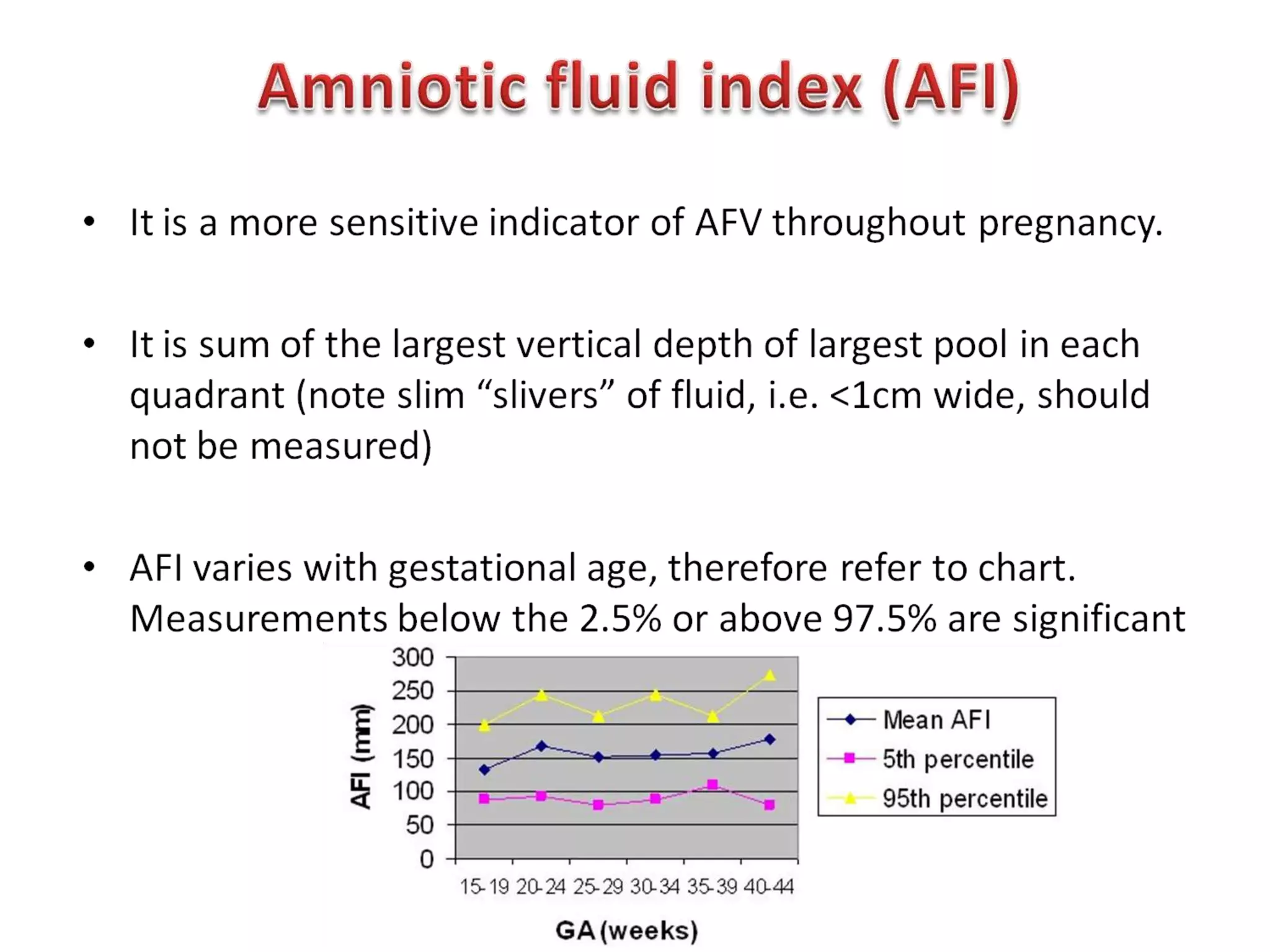
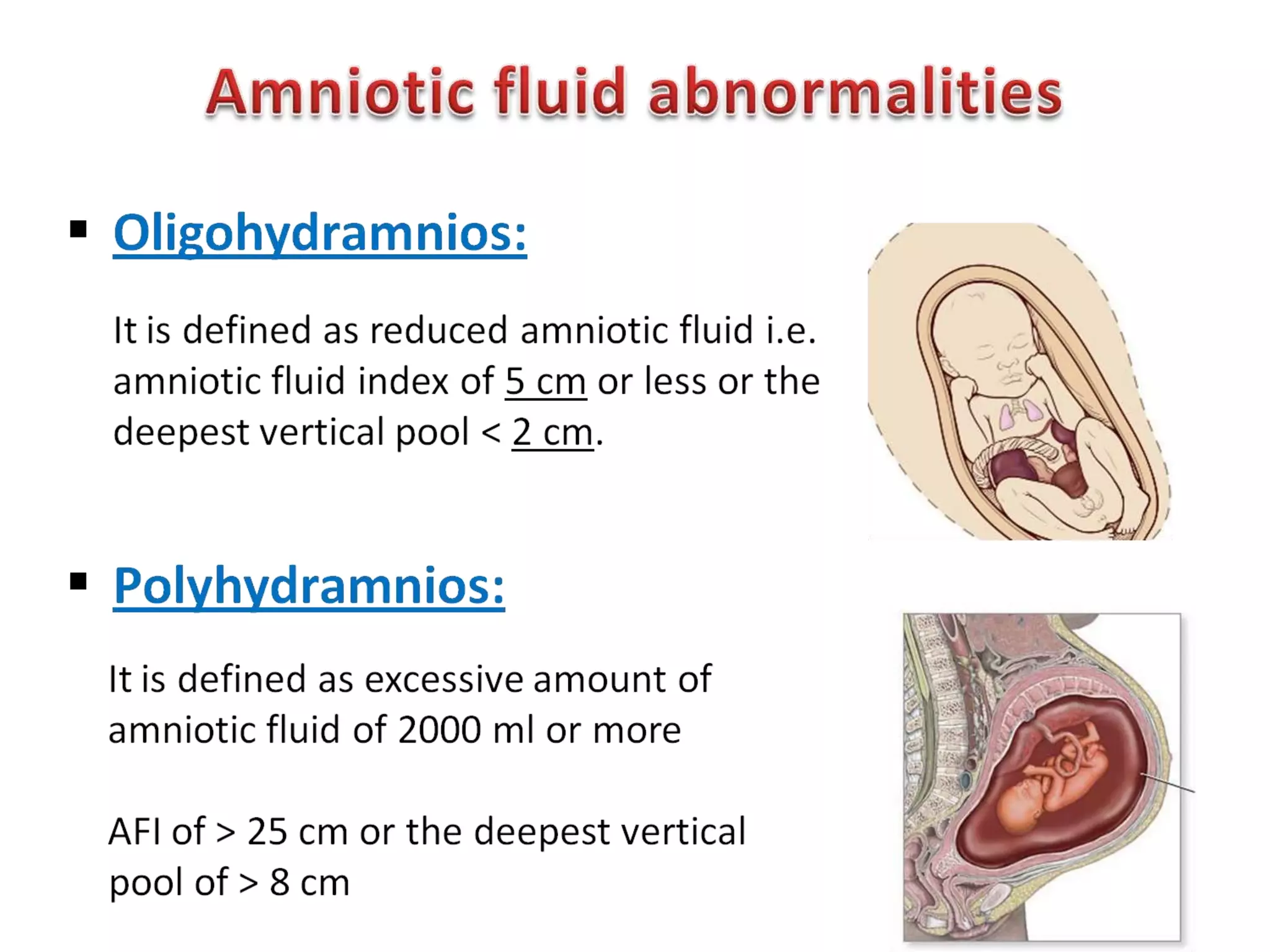
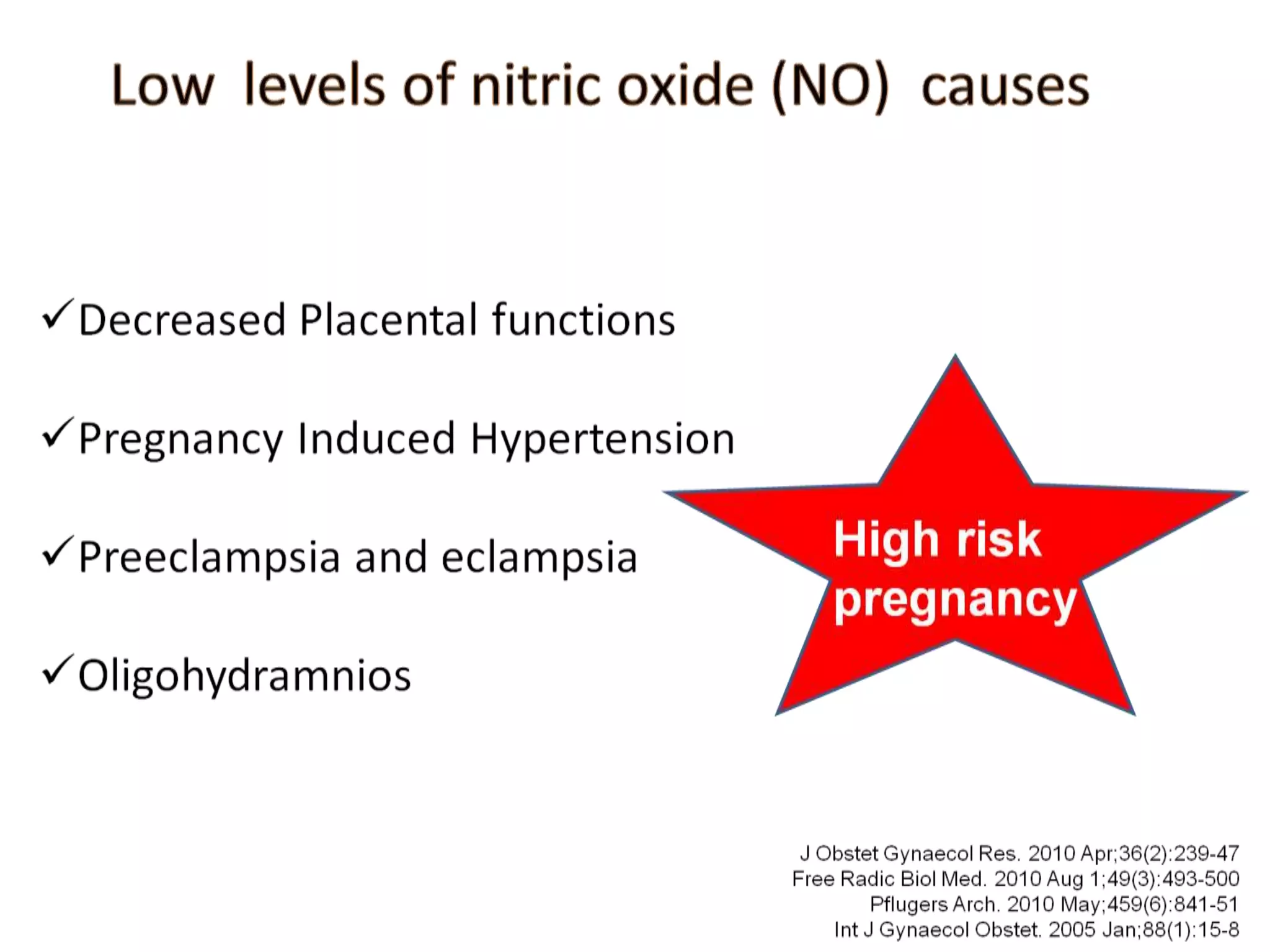
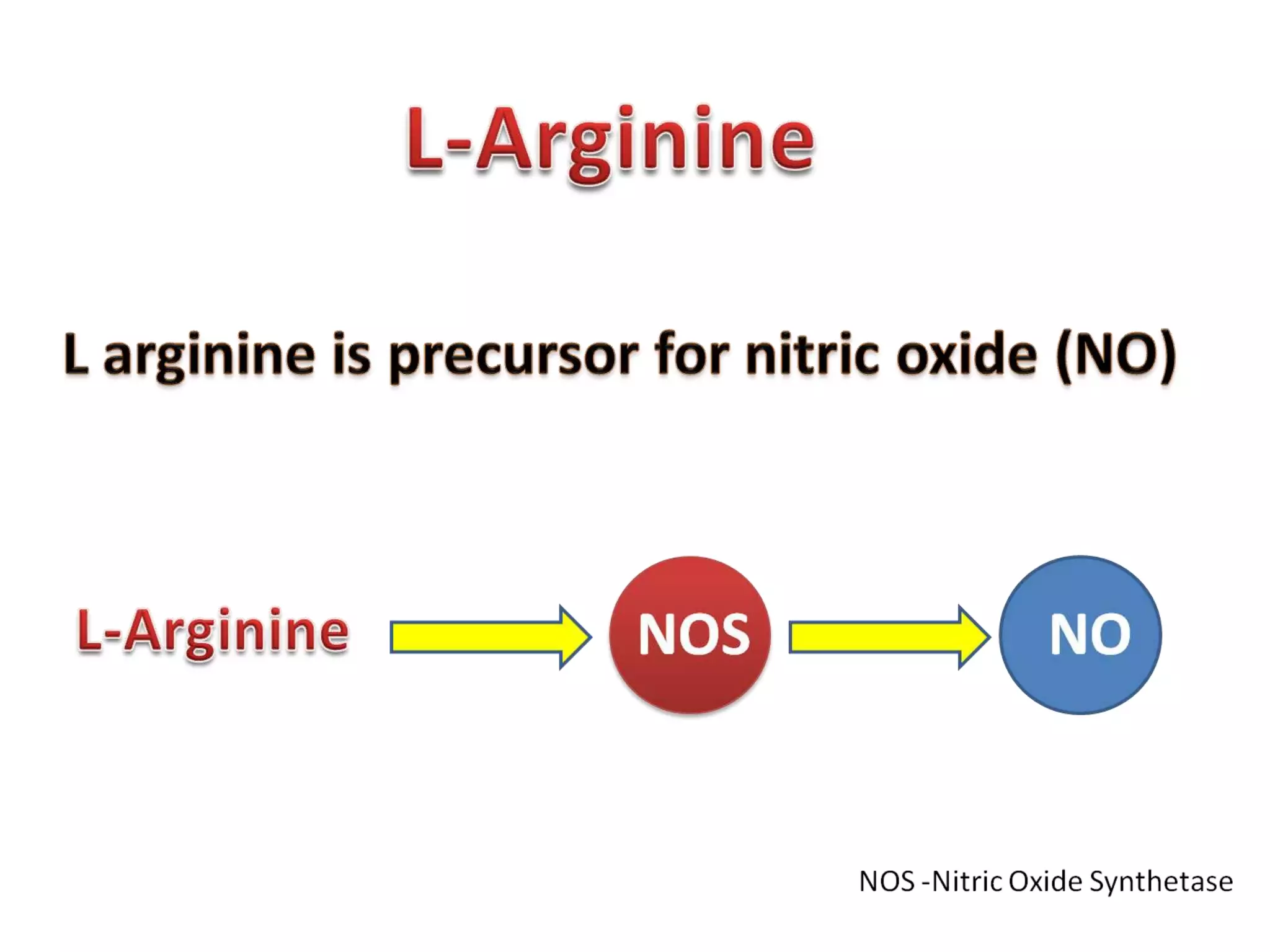
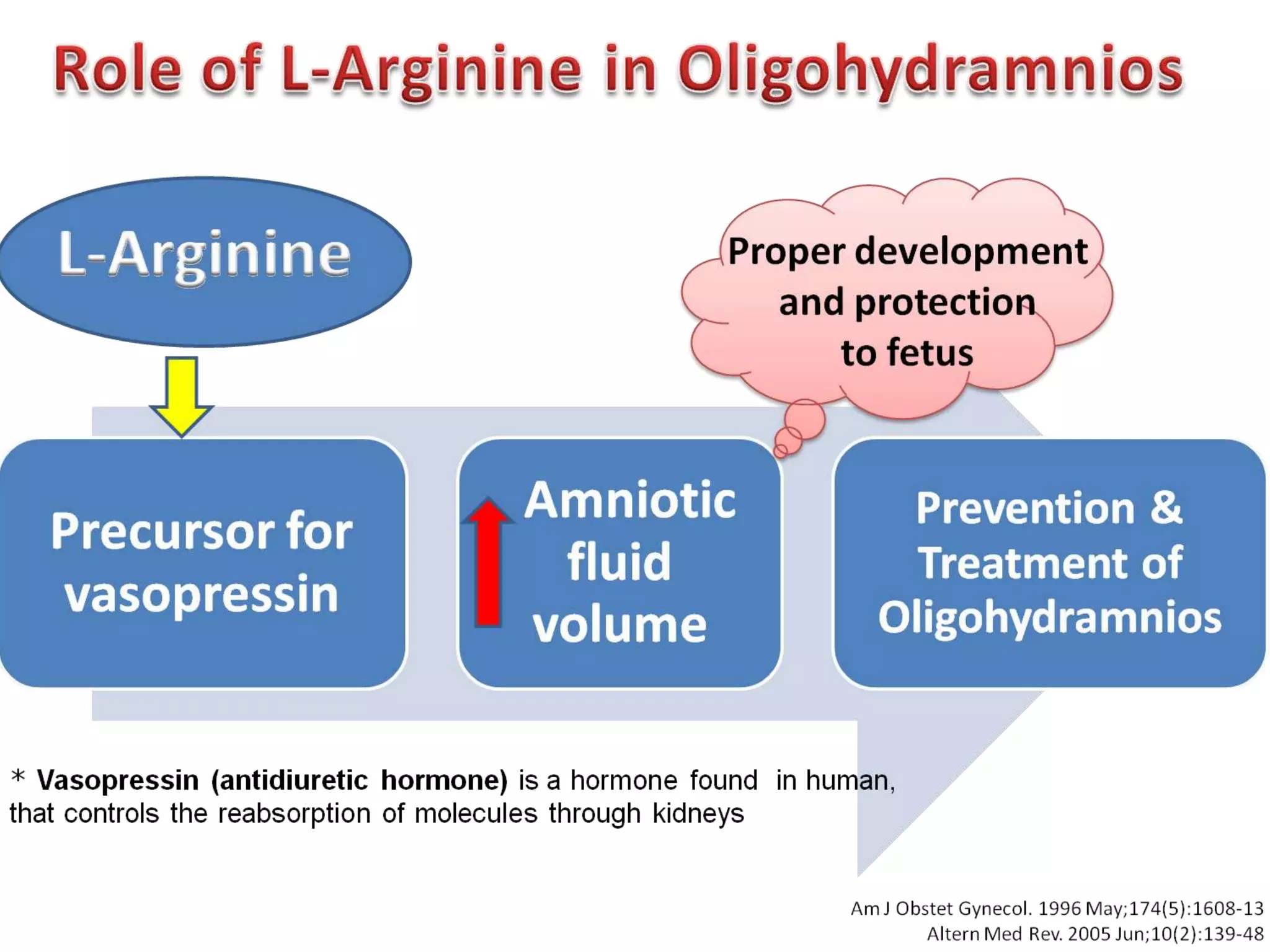
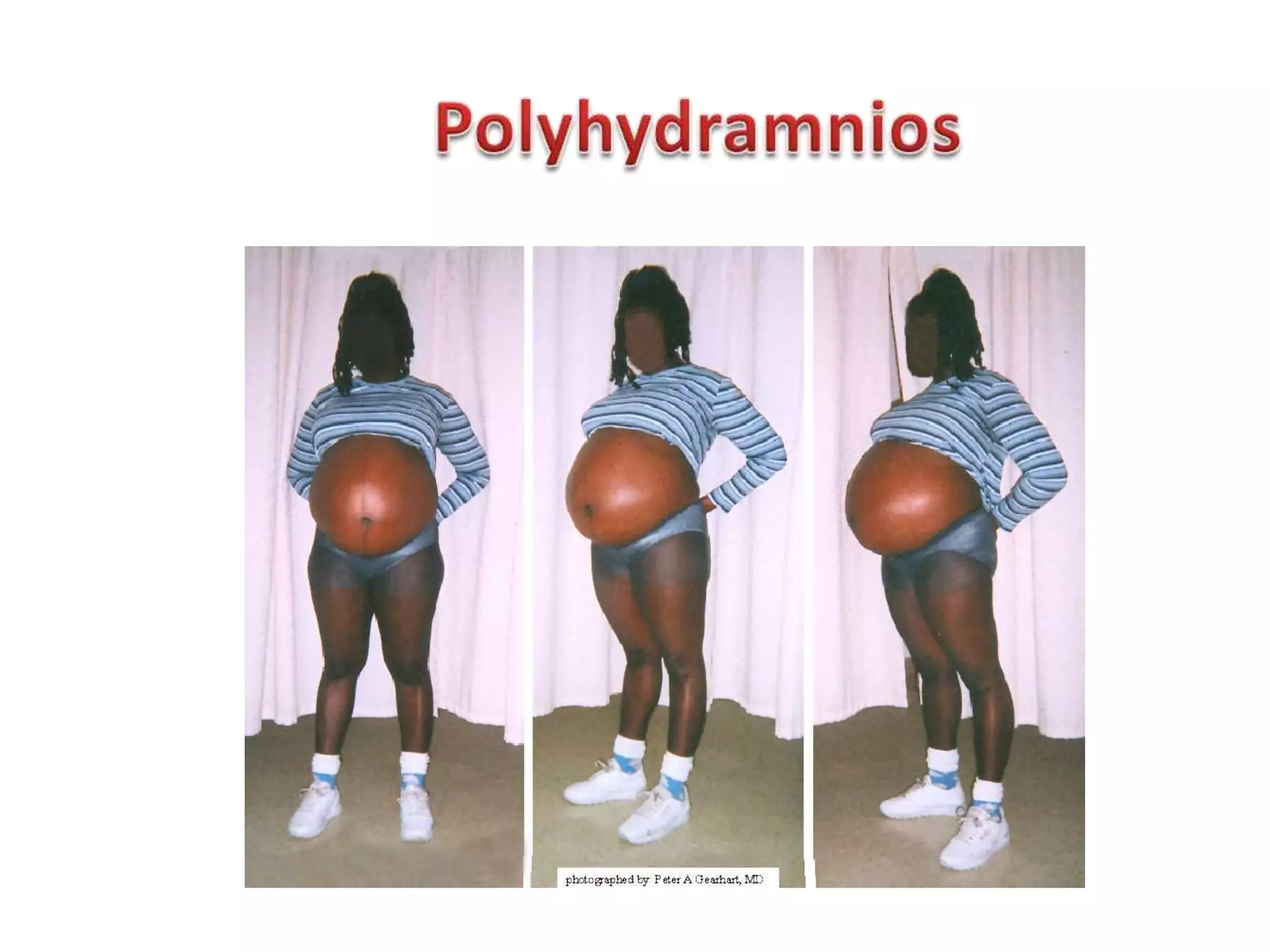
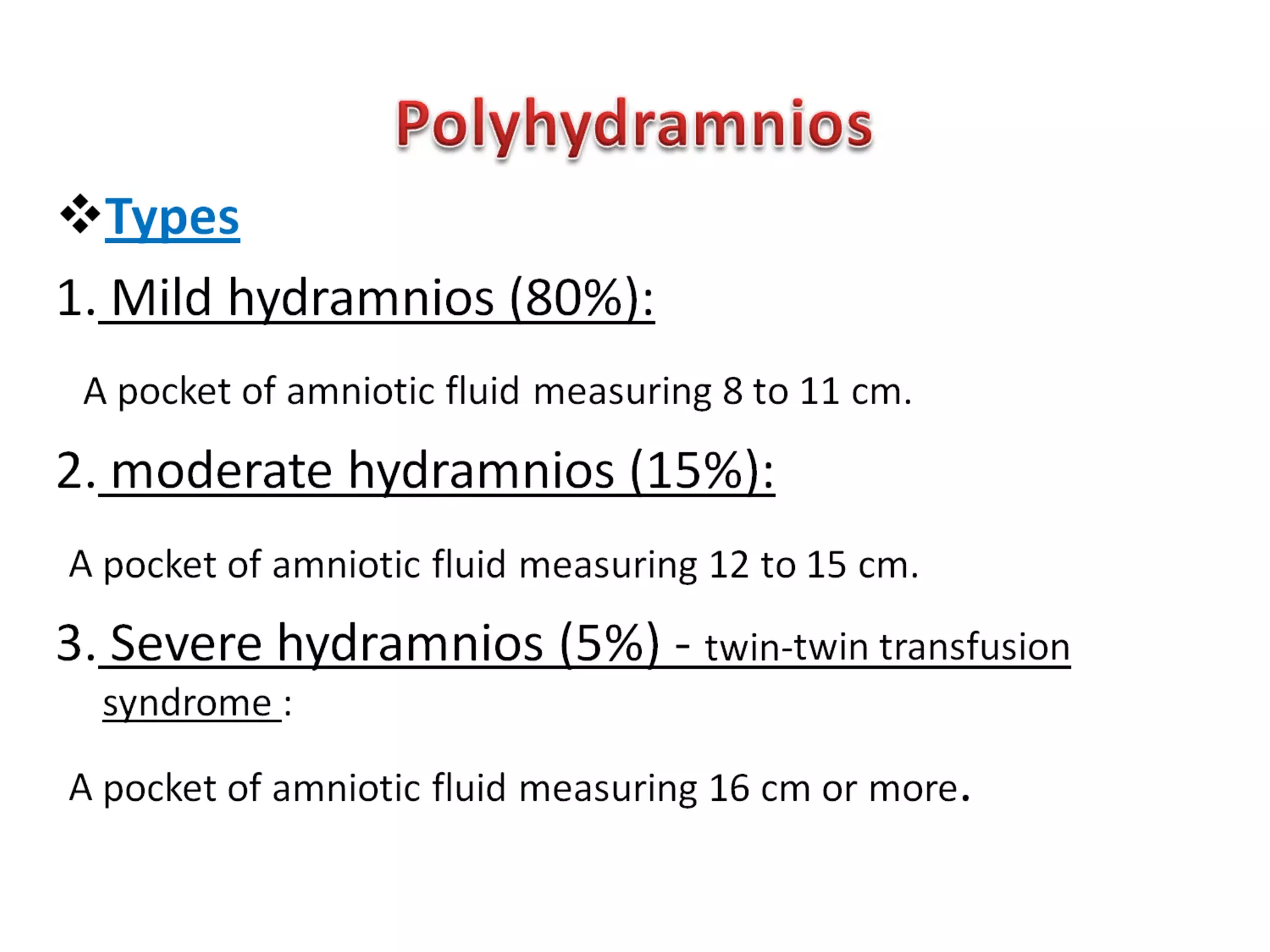
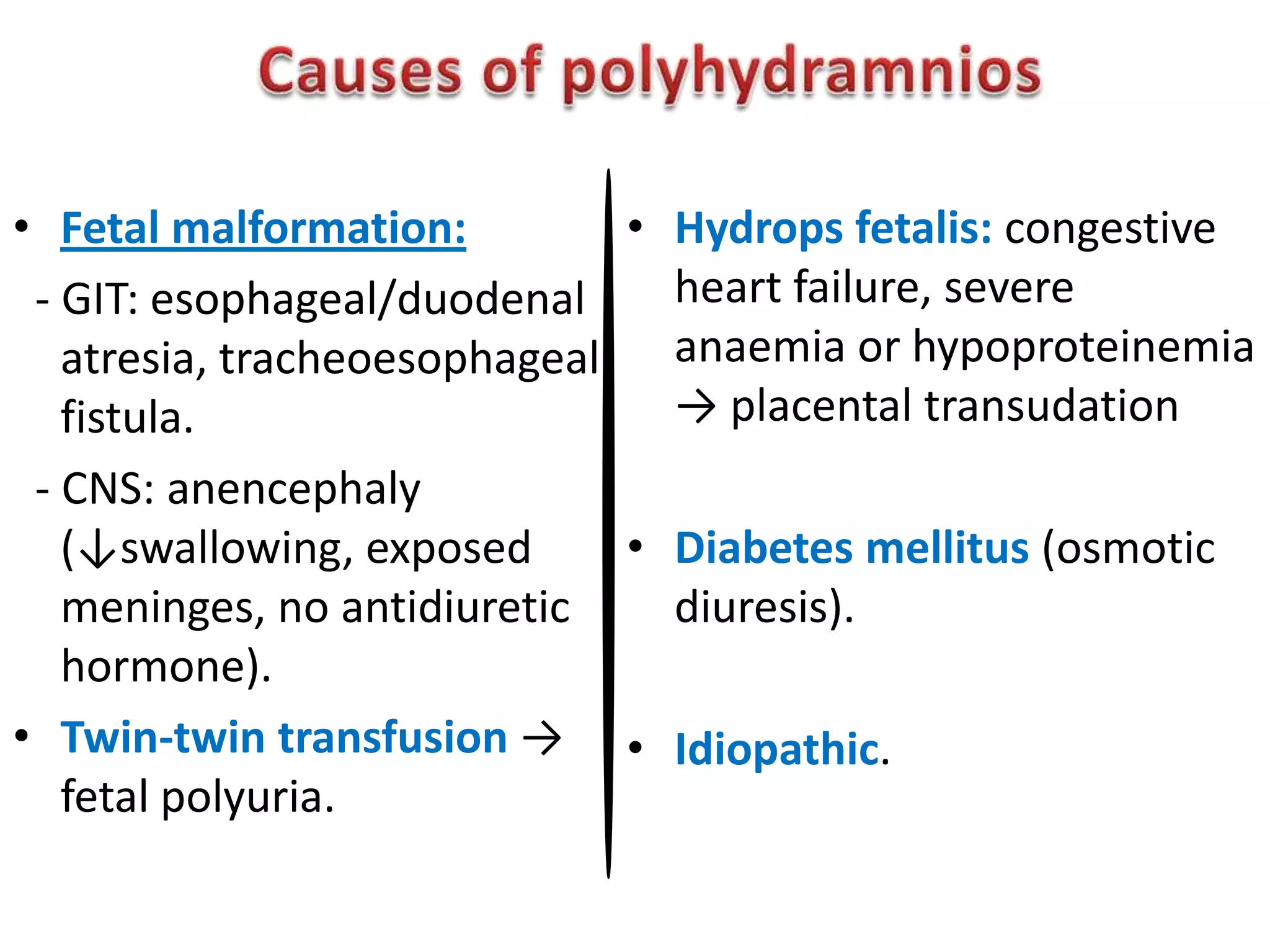
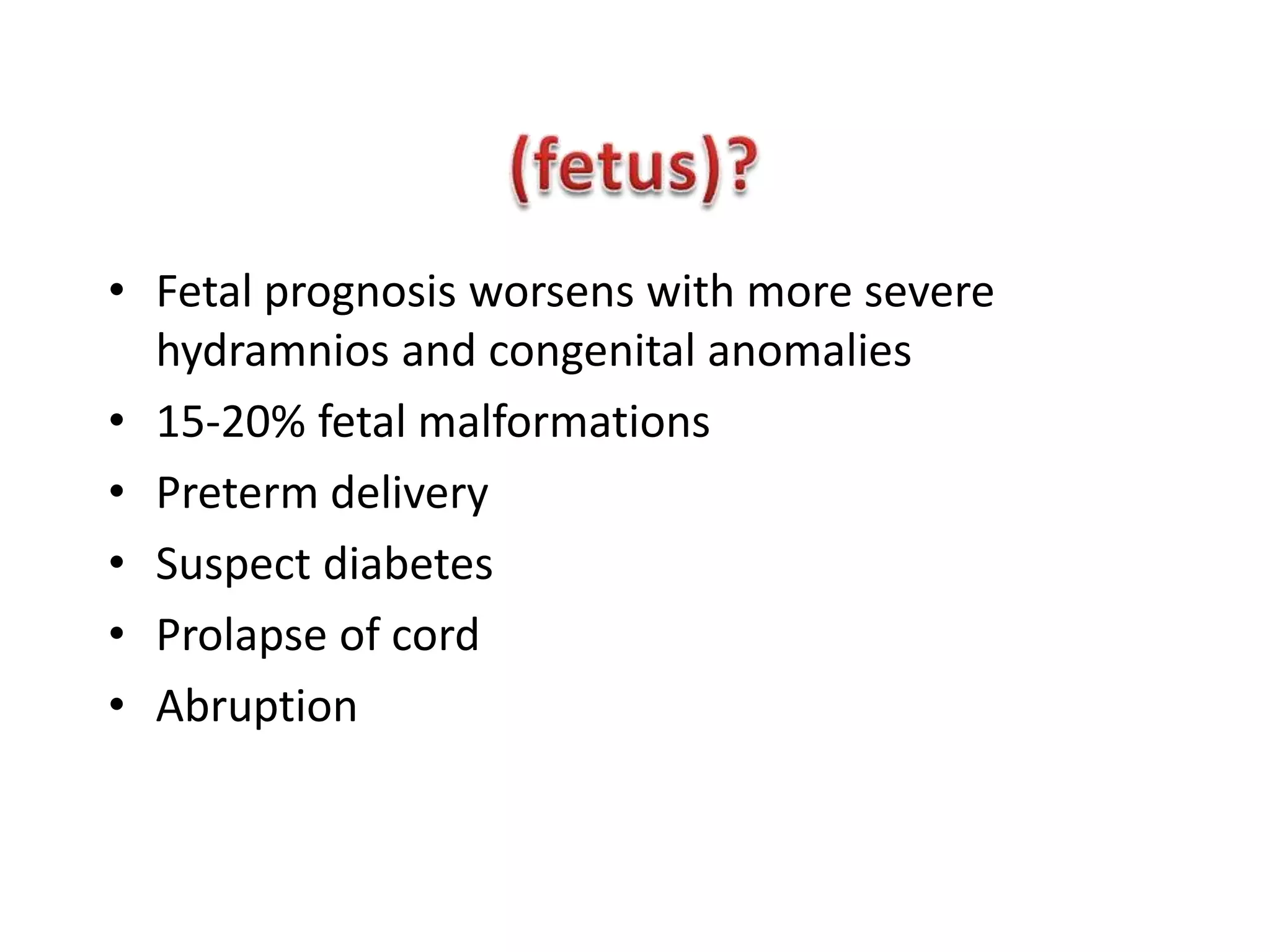
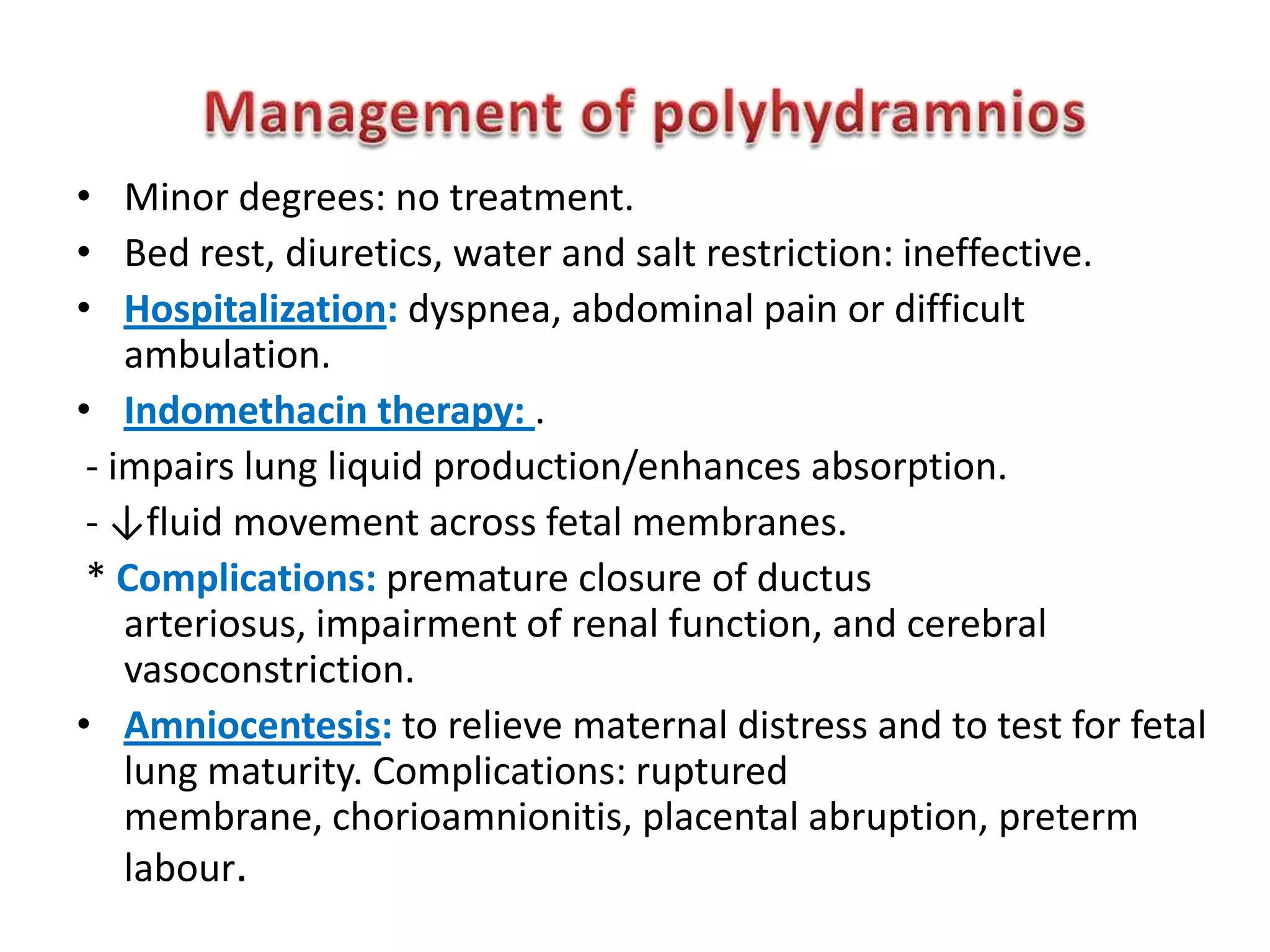
The document outlines various aspects of fetal assessment, including screening for malformations, assessments of fetal well-being, and amniotic fluid measurements. It discusses maternal and placental causes of complications, risks associated with abnormalities, and potential treatments for managing conditions like hydramnios and fetal distress. Key interventions include ultrasound diagnostics, amniocentesis, and medication to adjust amniotic fluid levels.