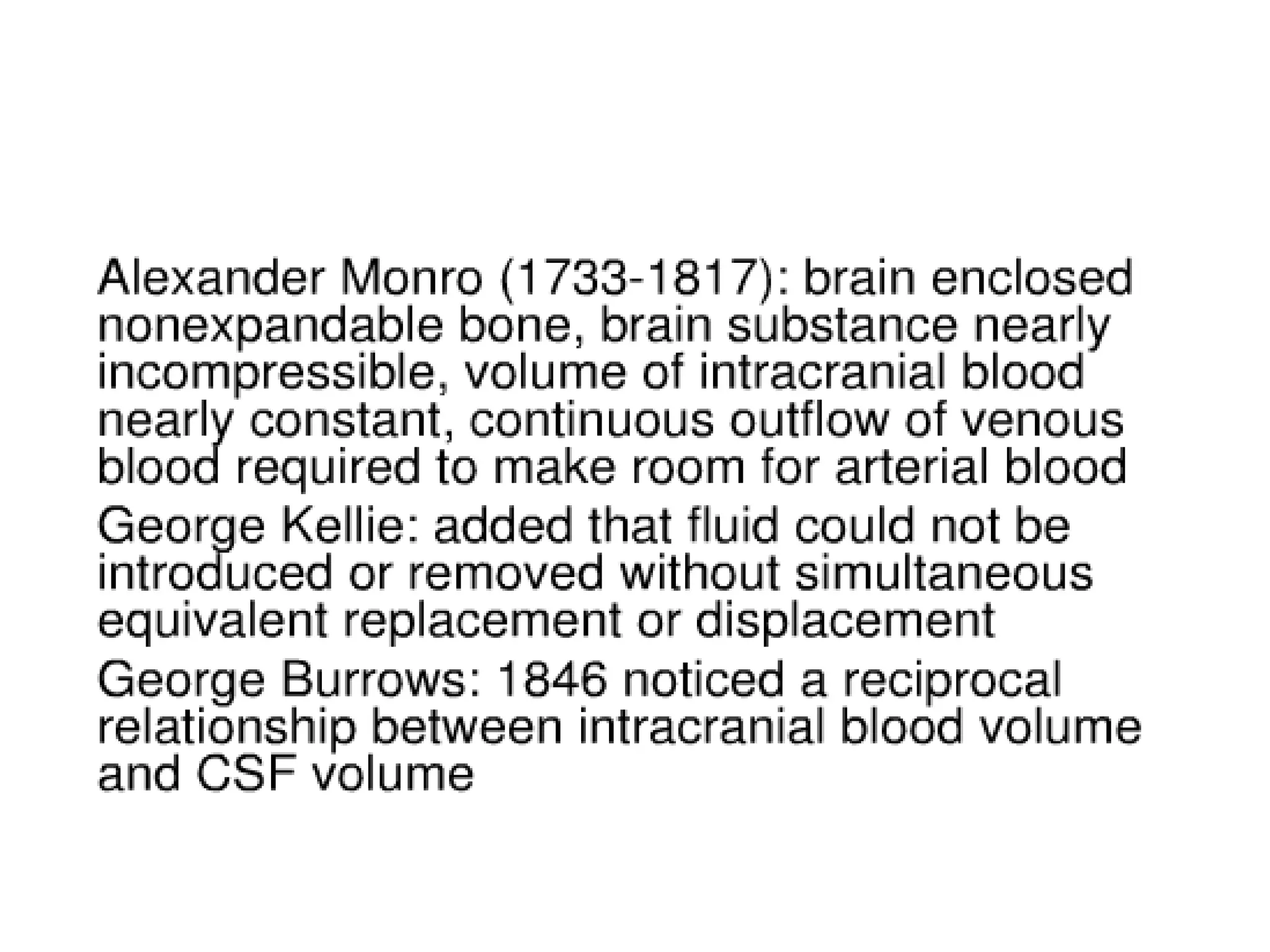
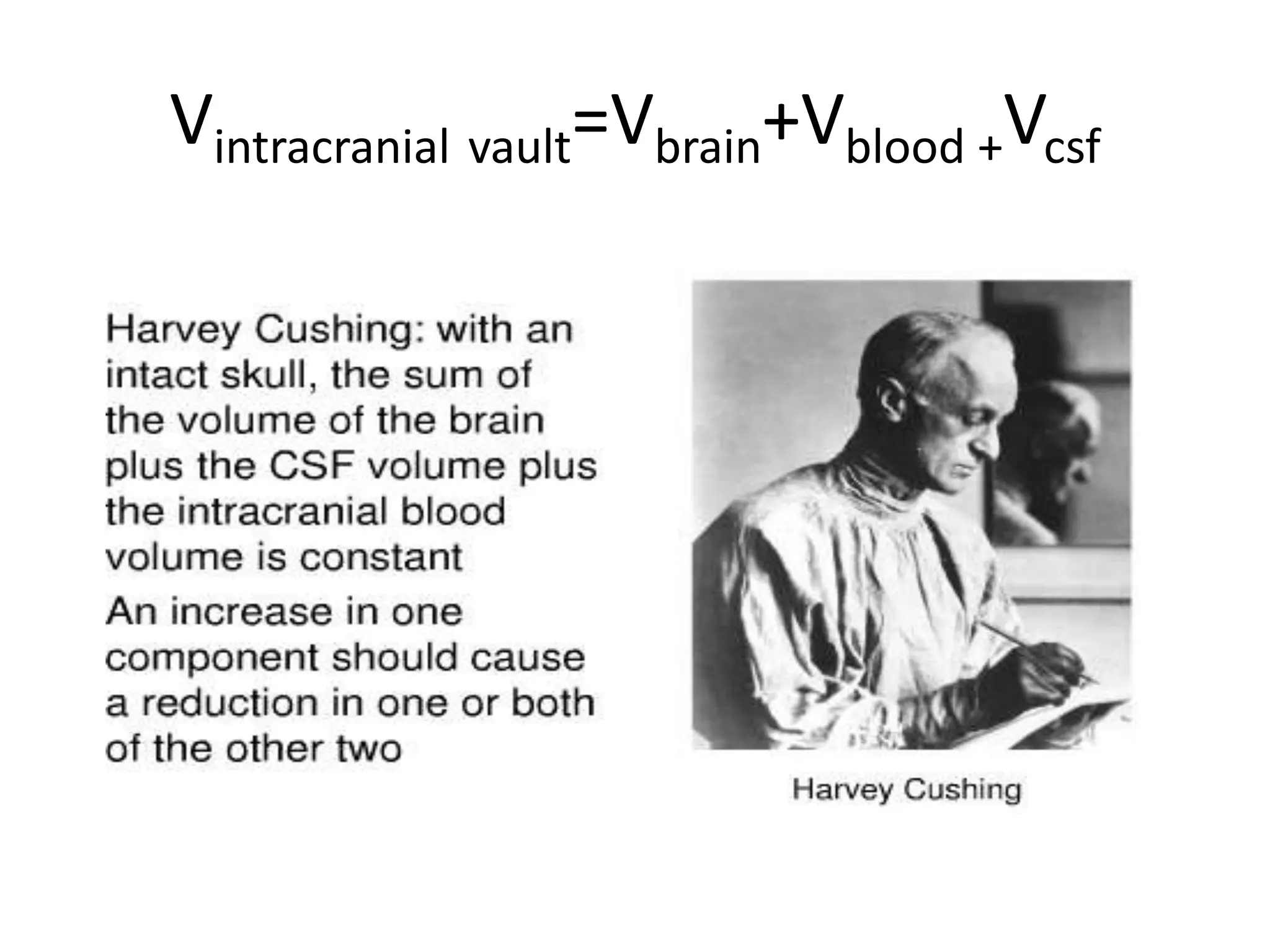
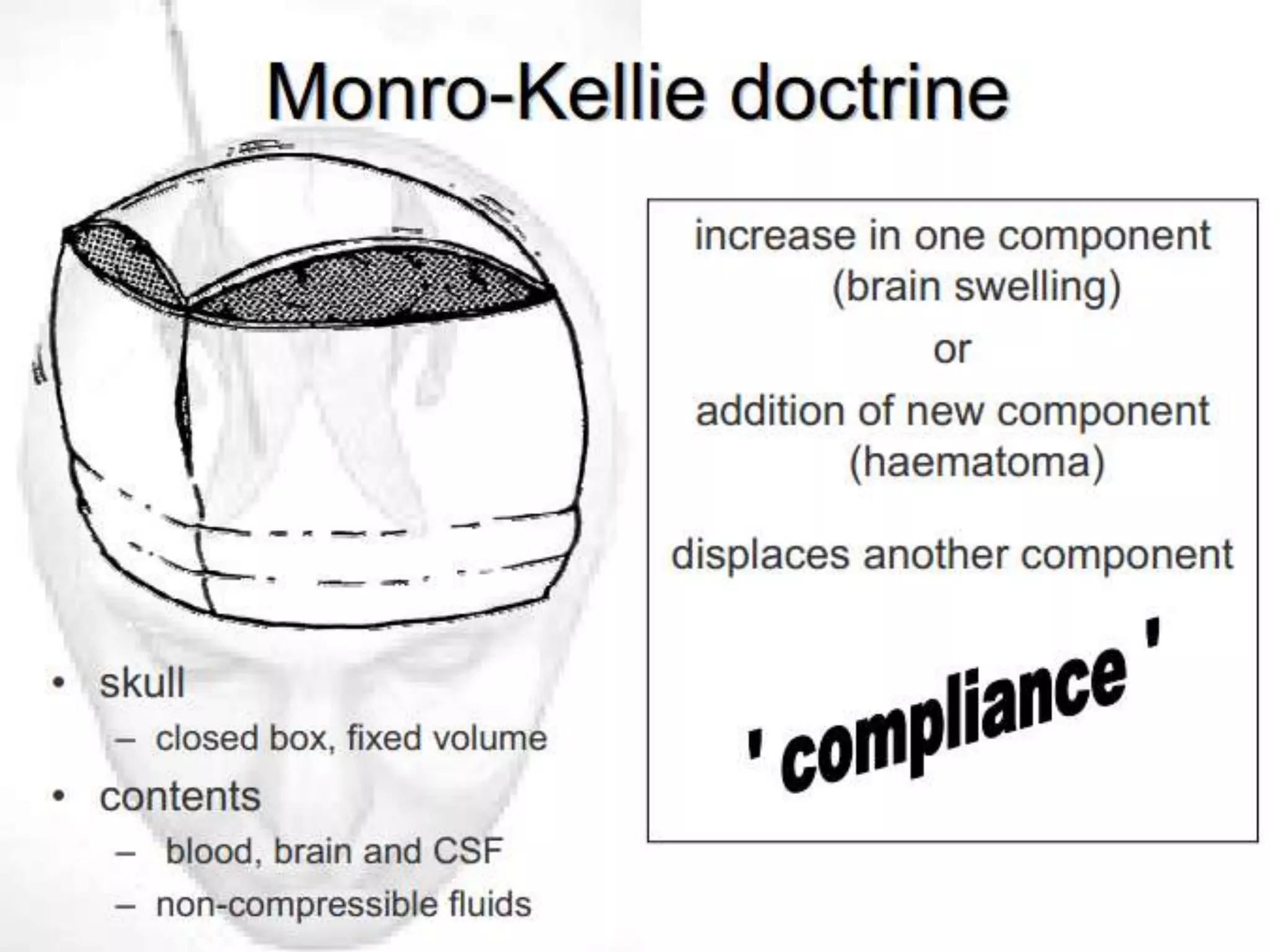
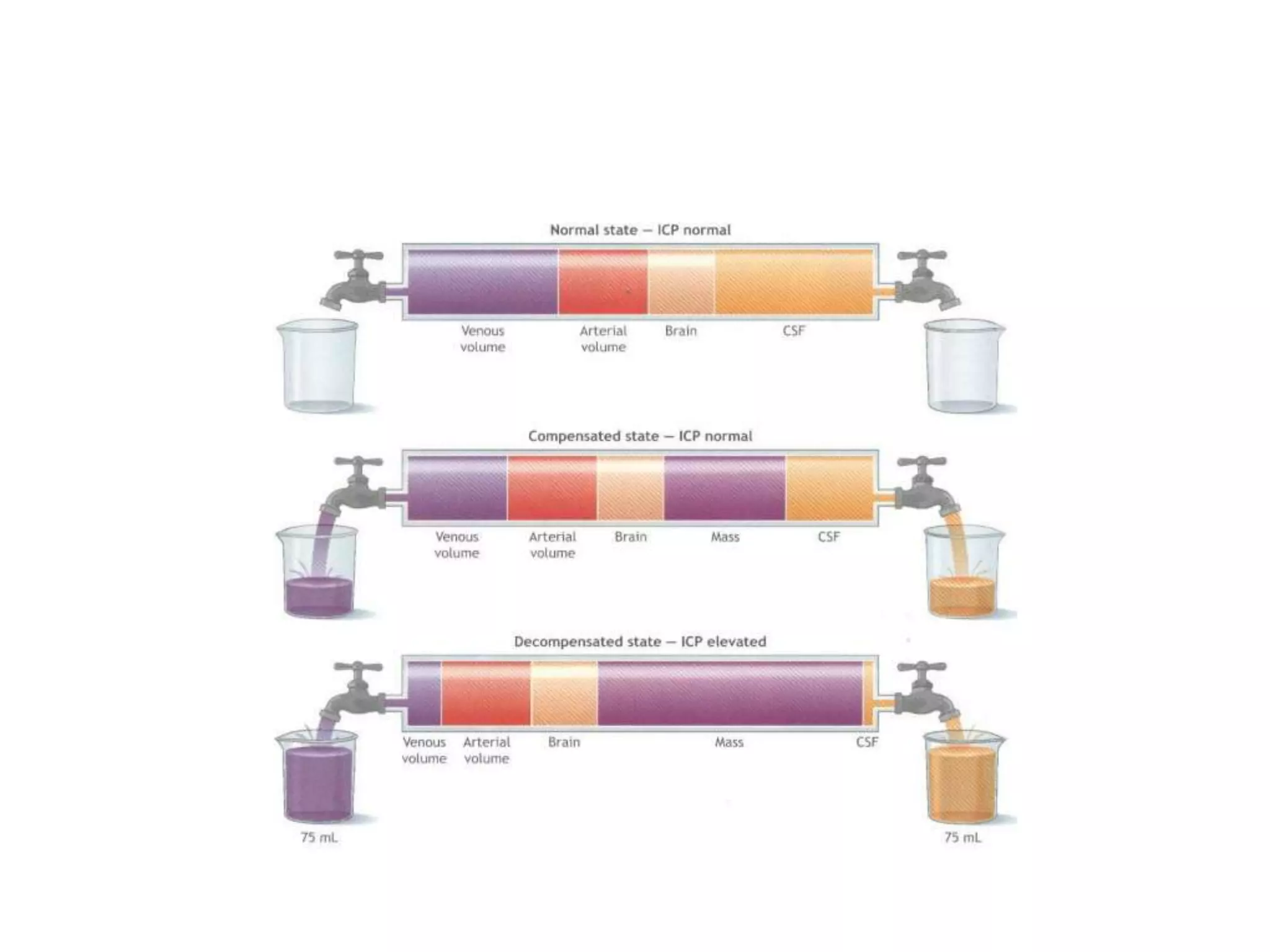
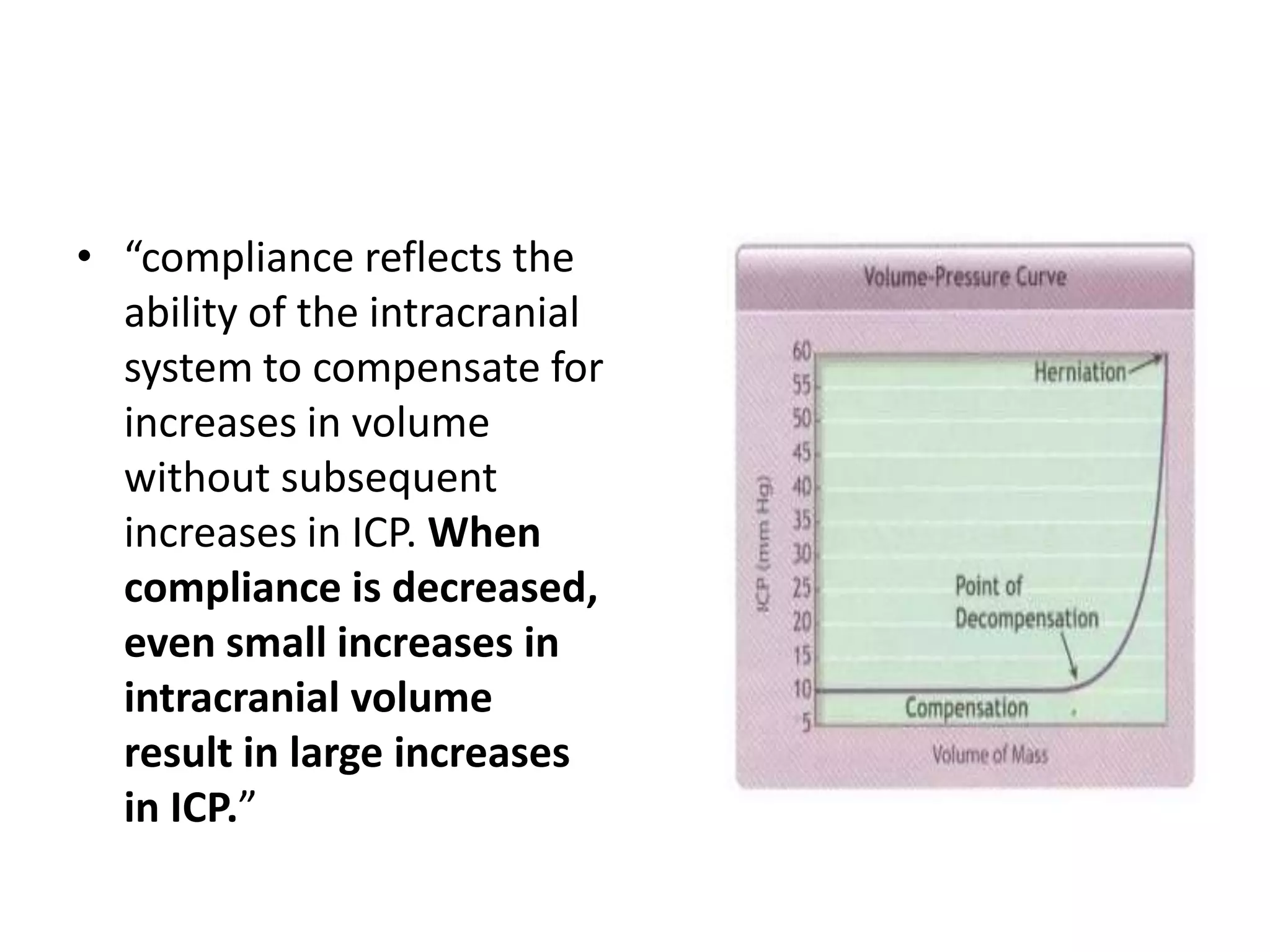
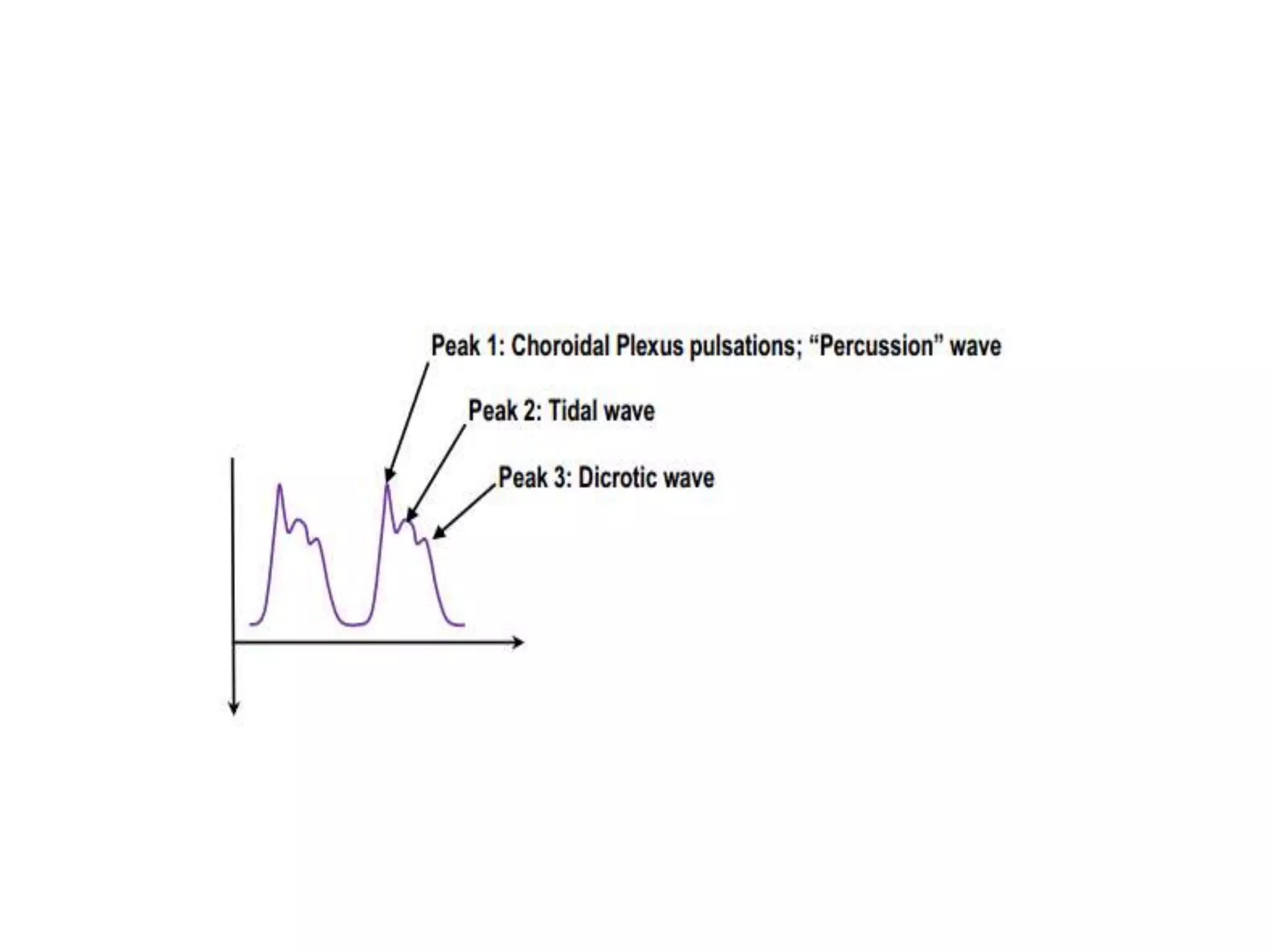
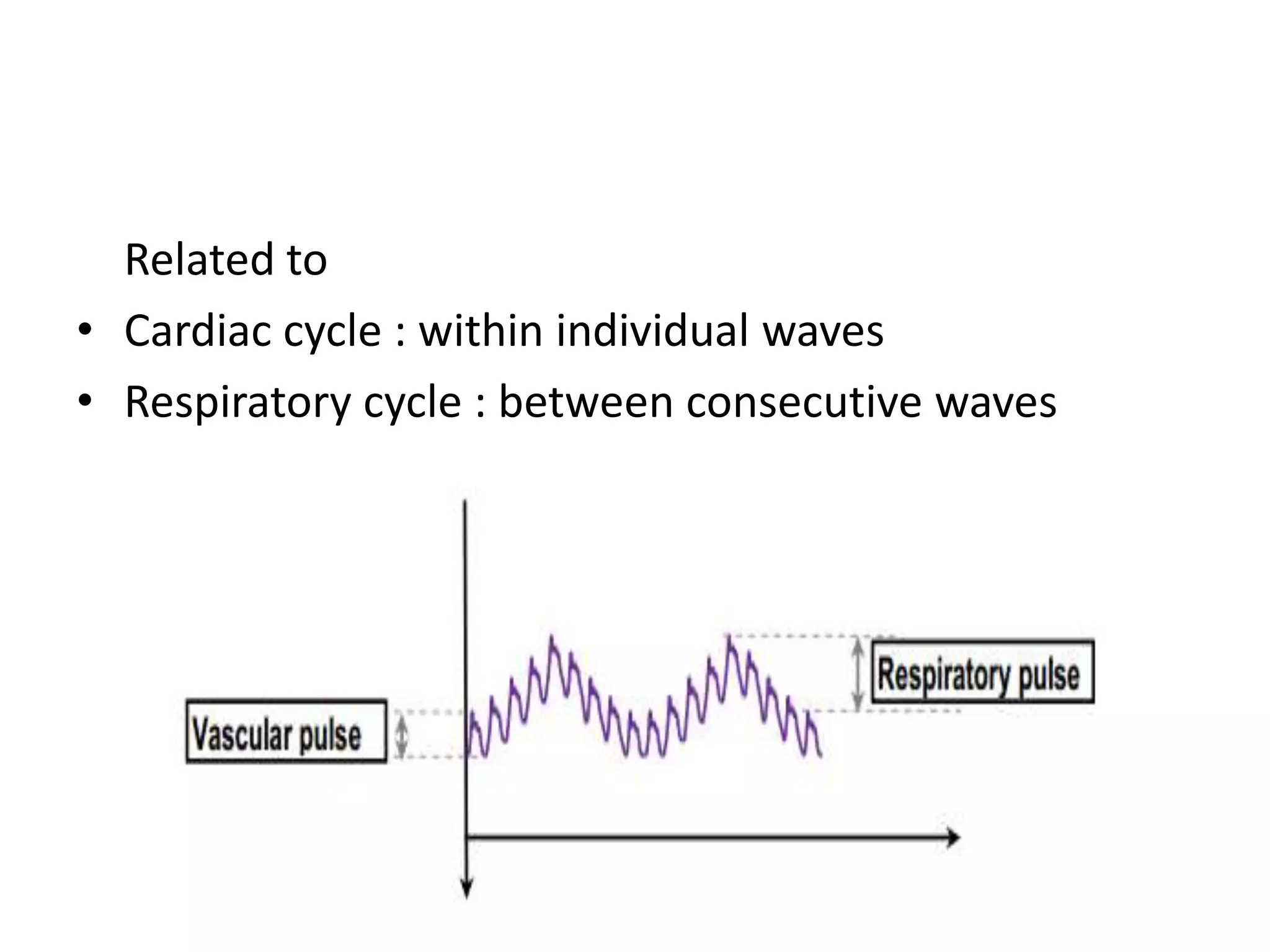
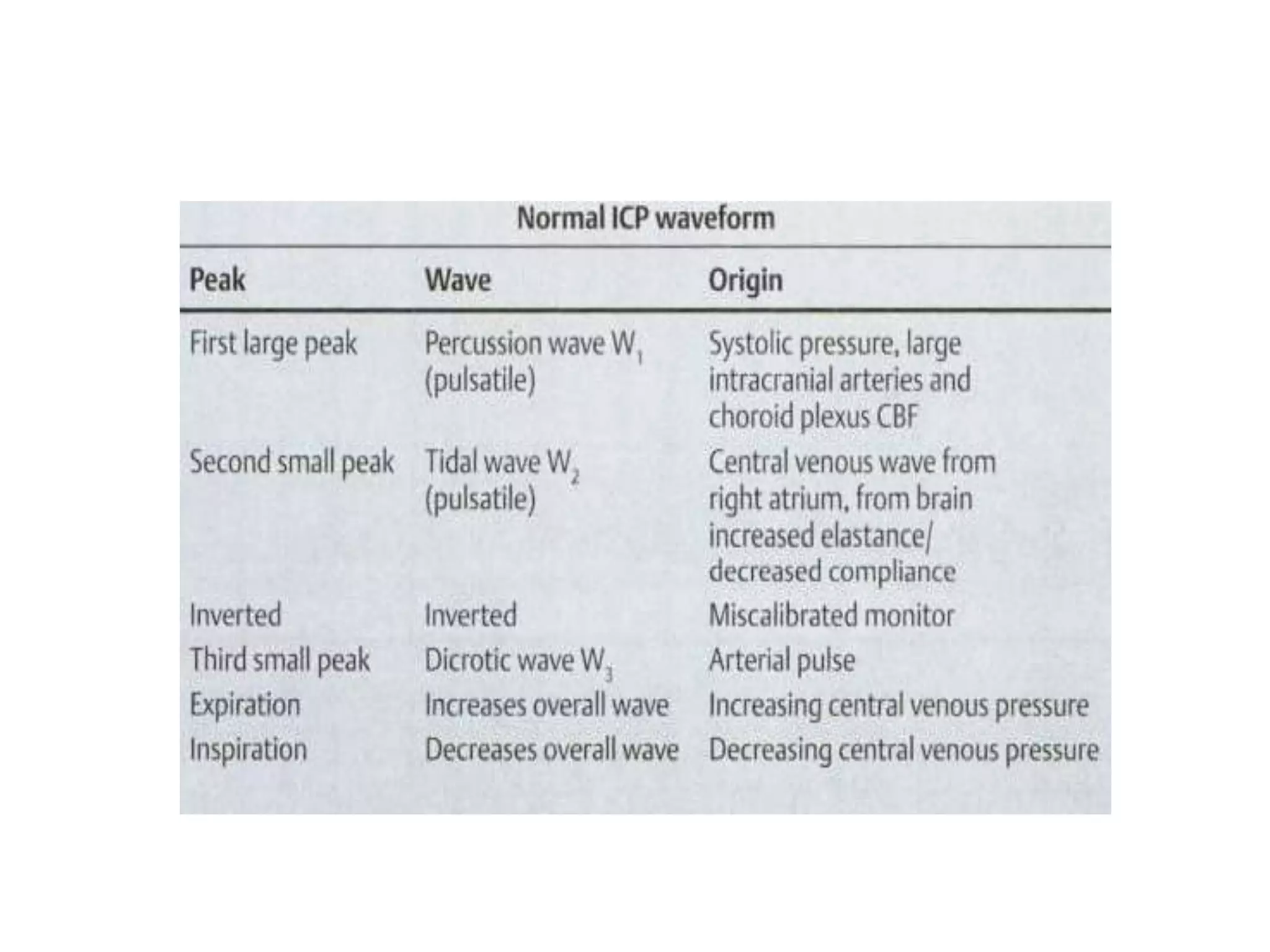
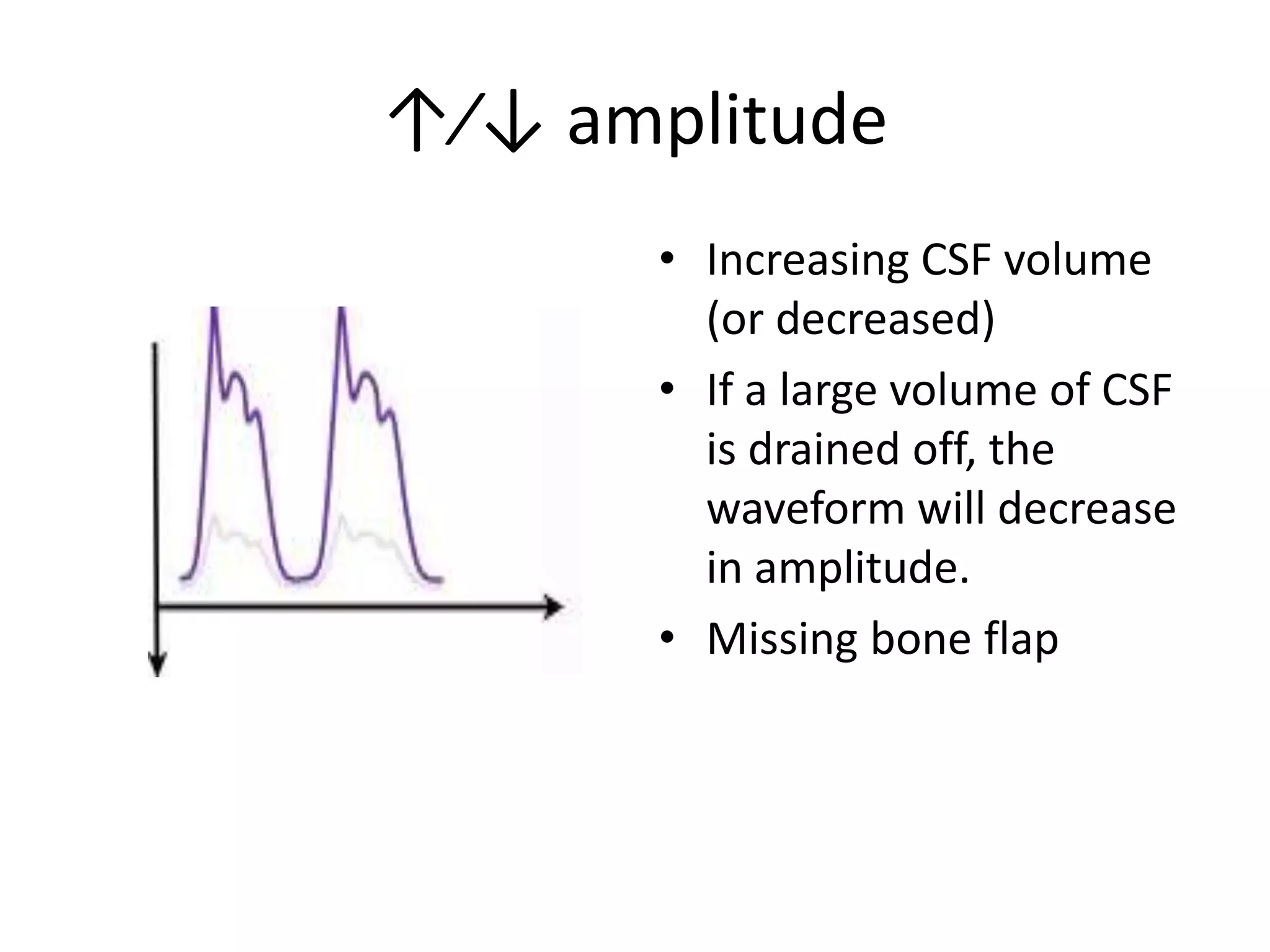
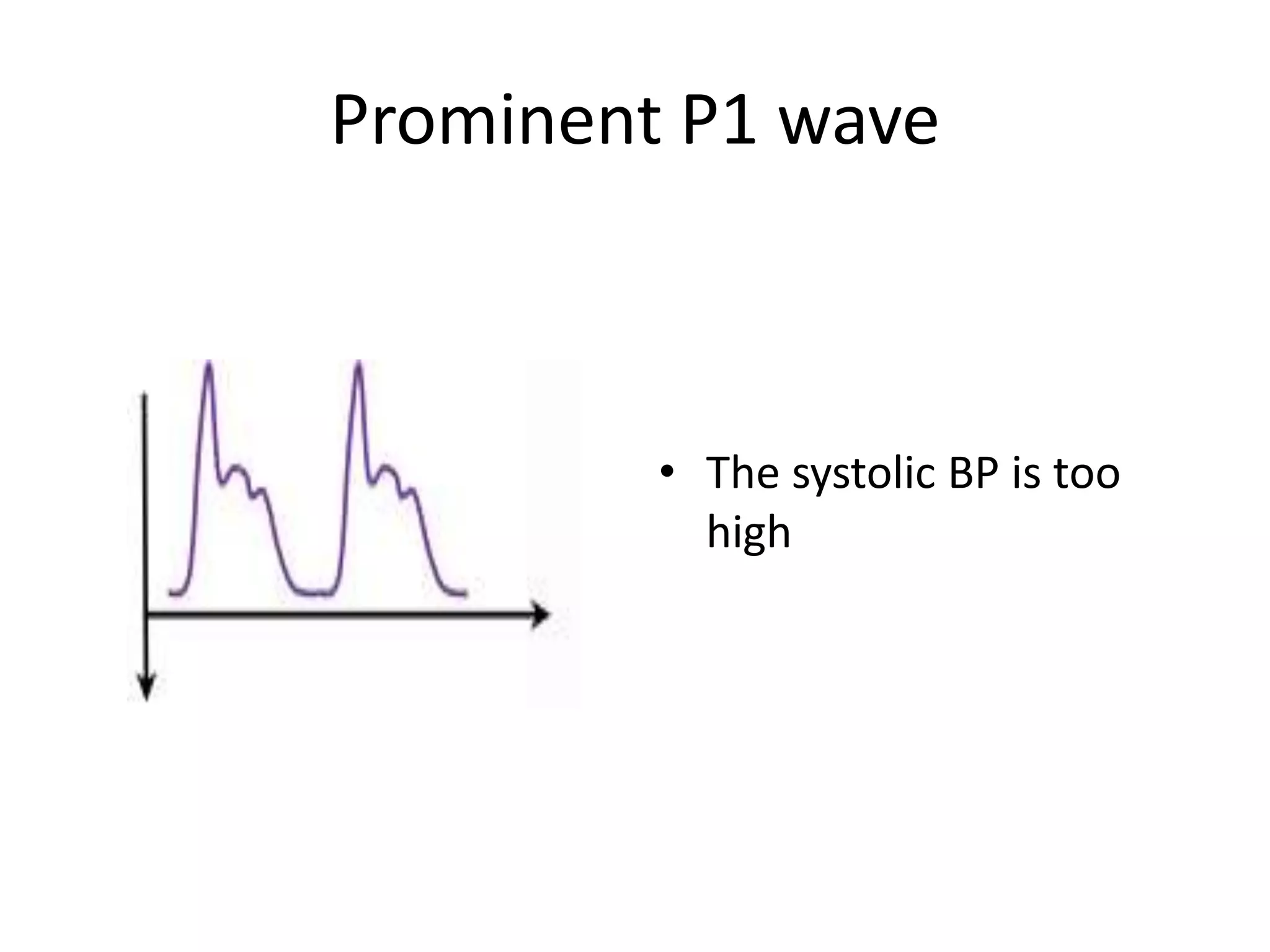
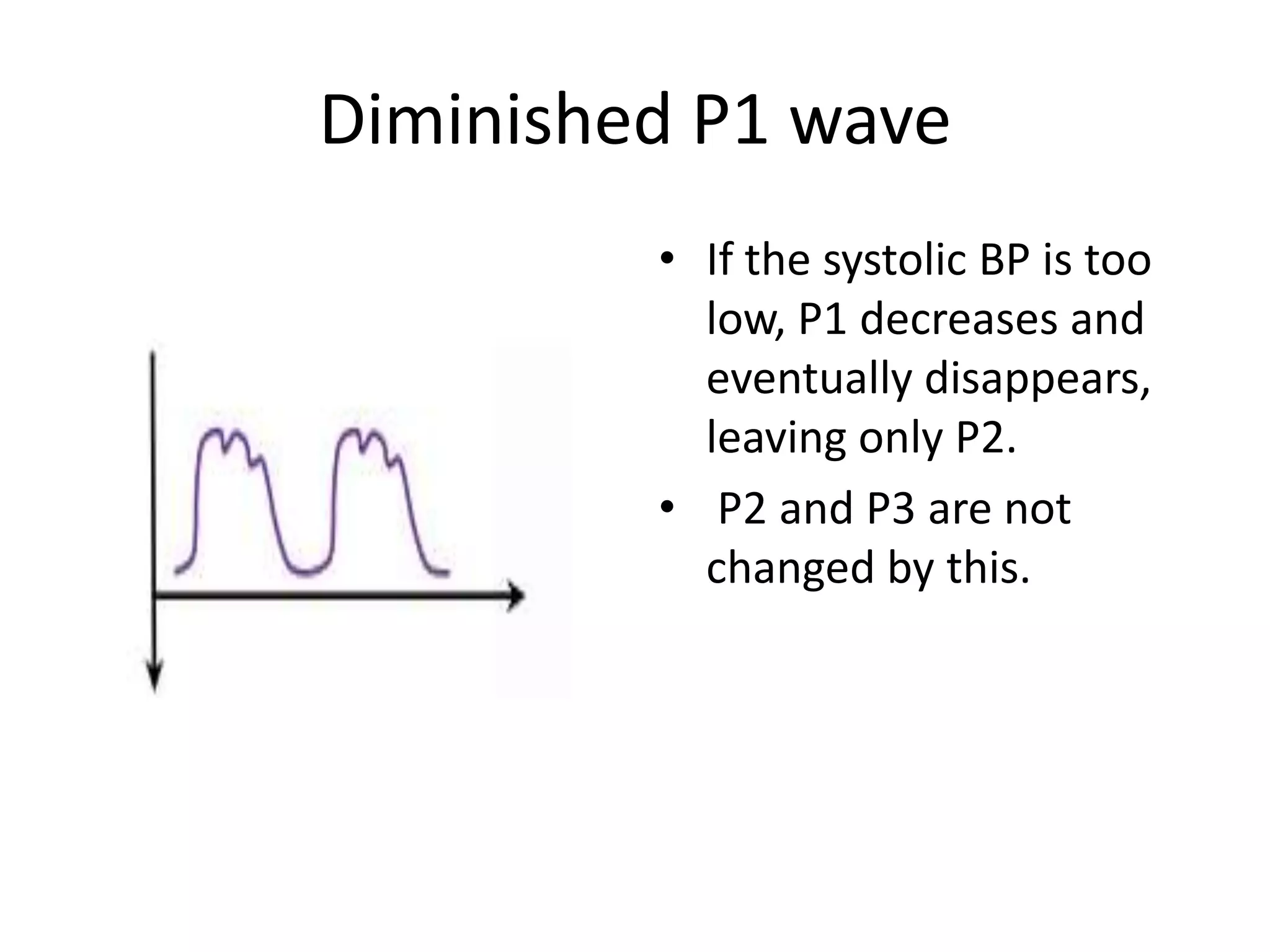
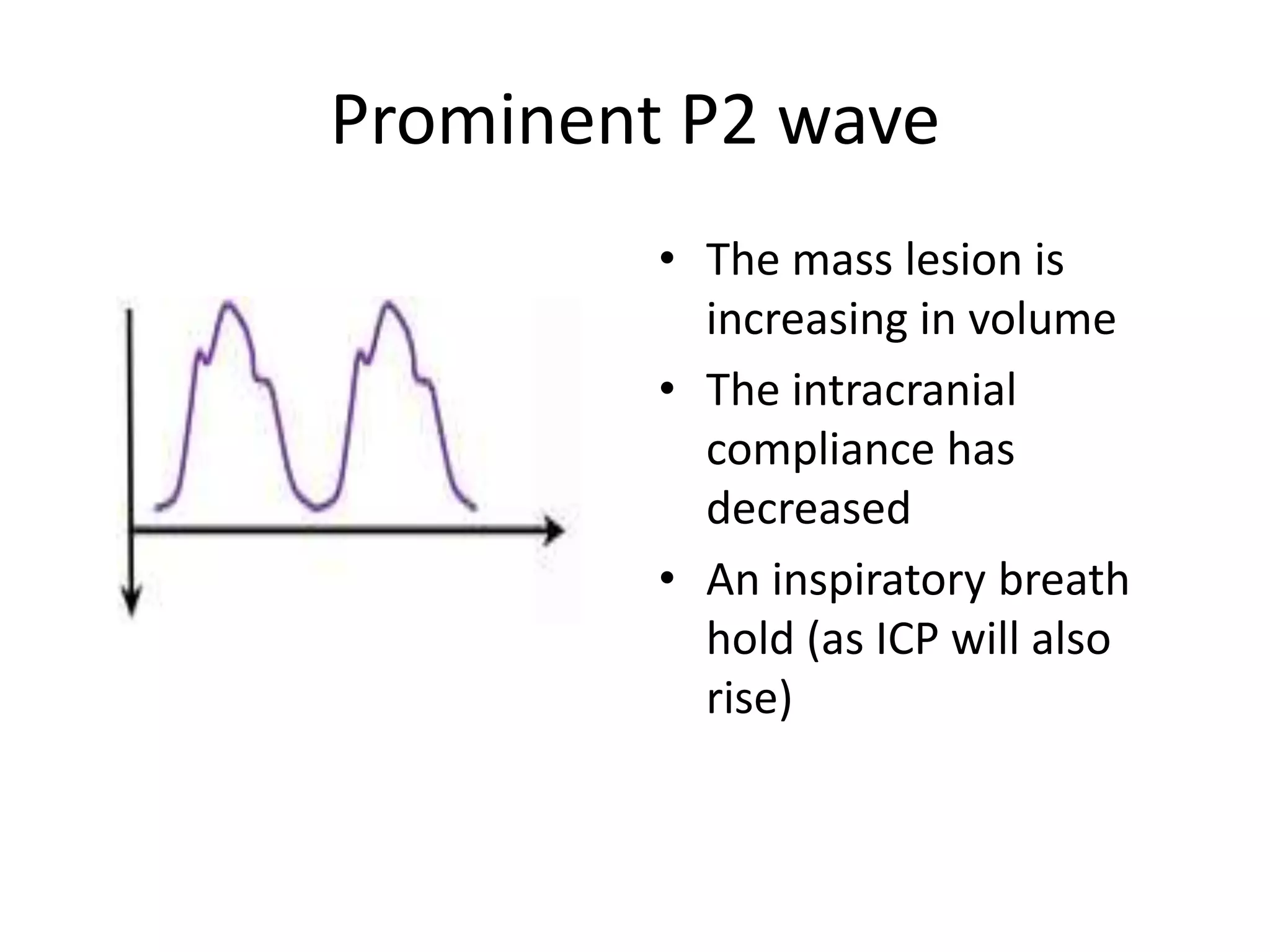
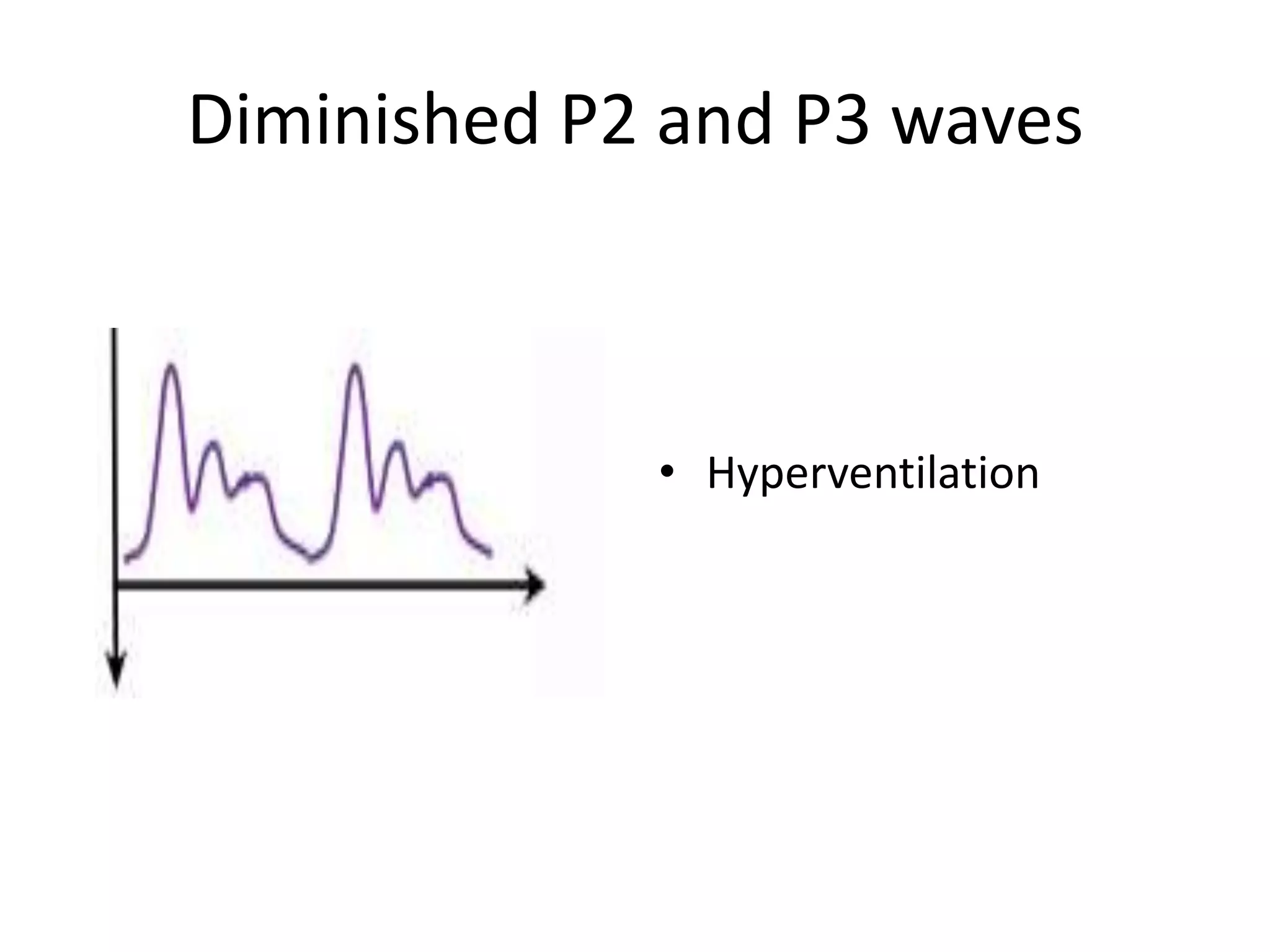
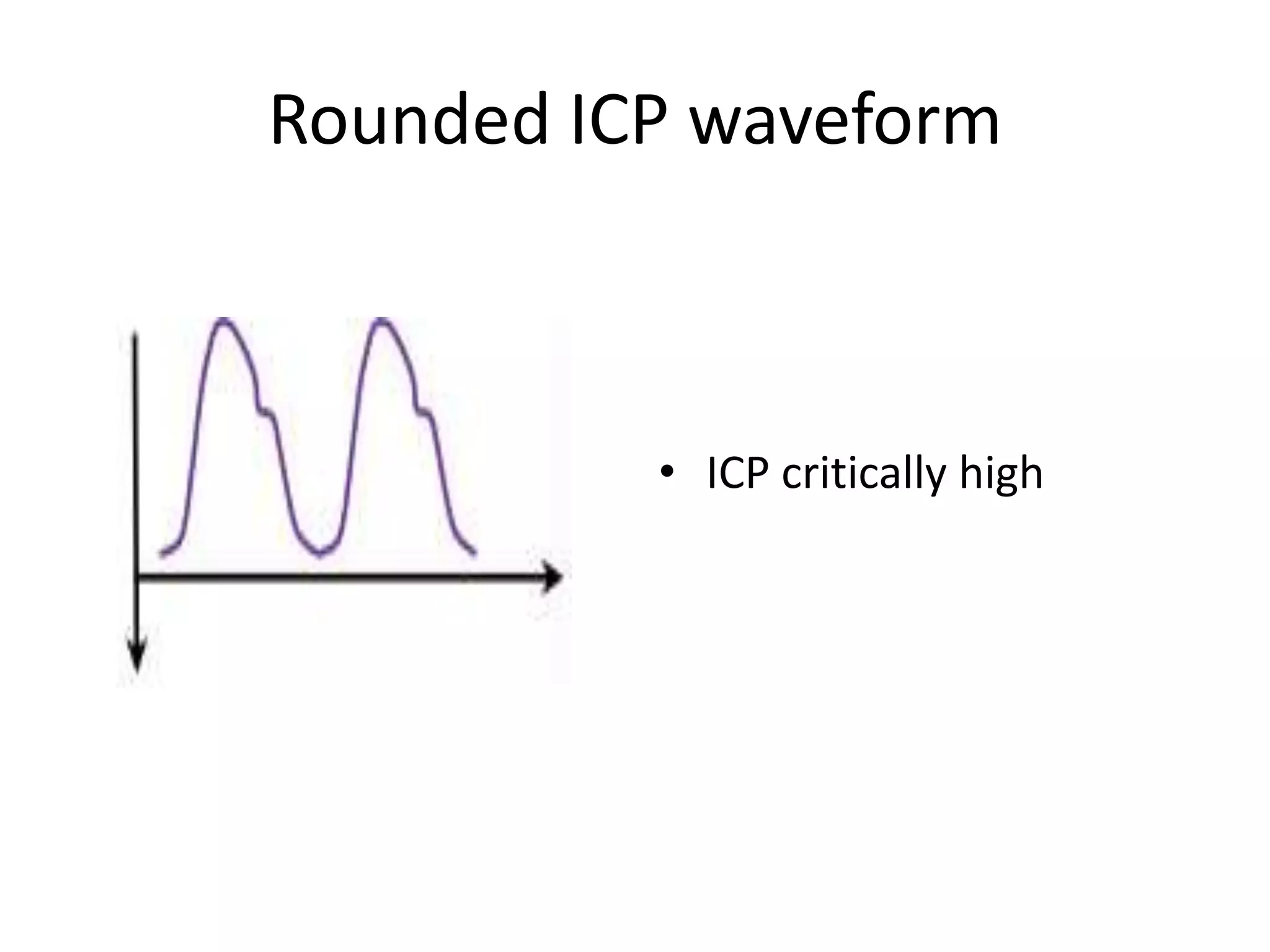
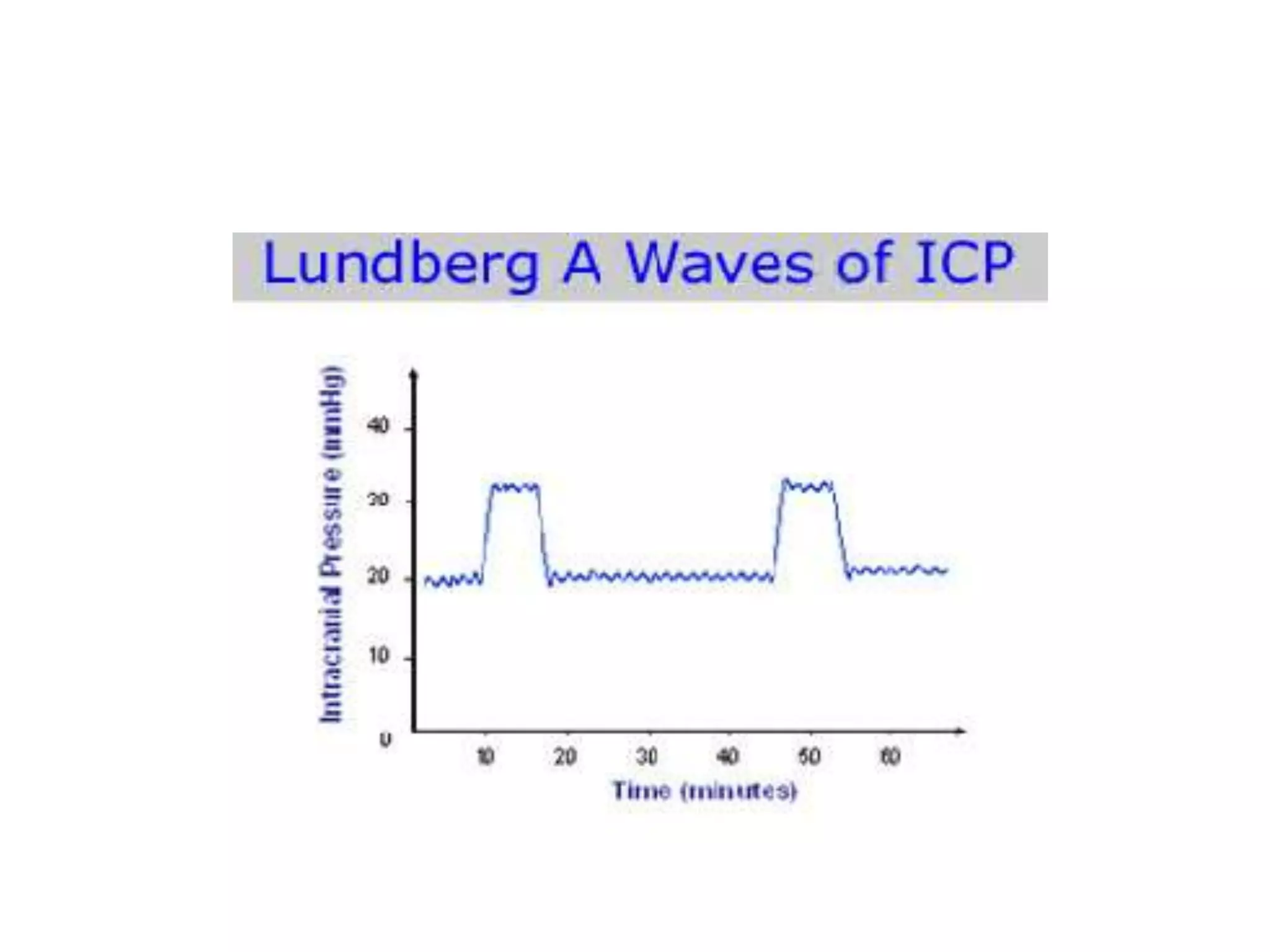
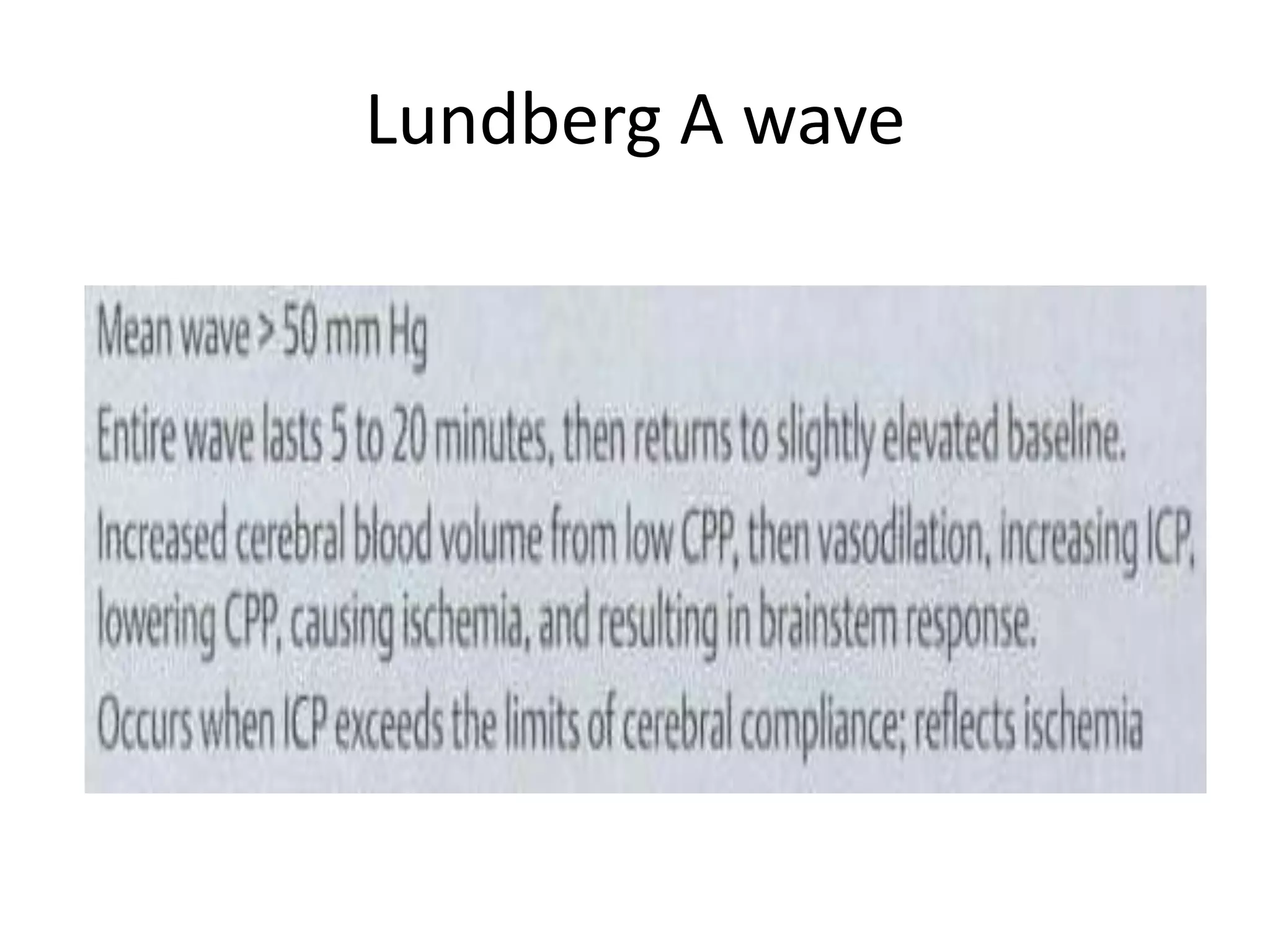
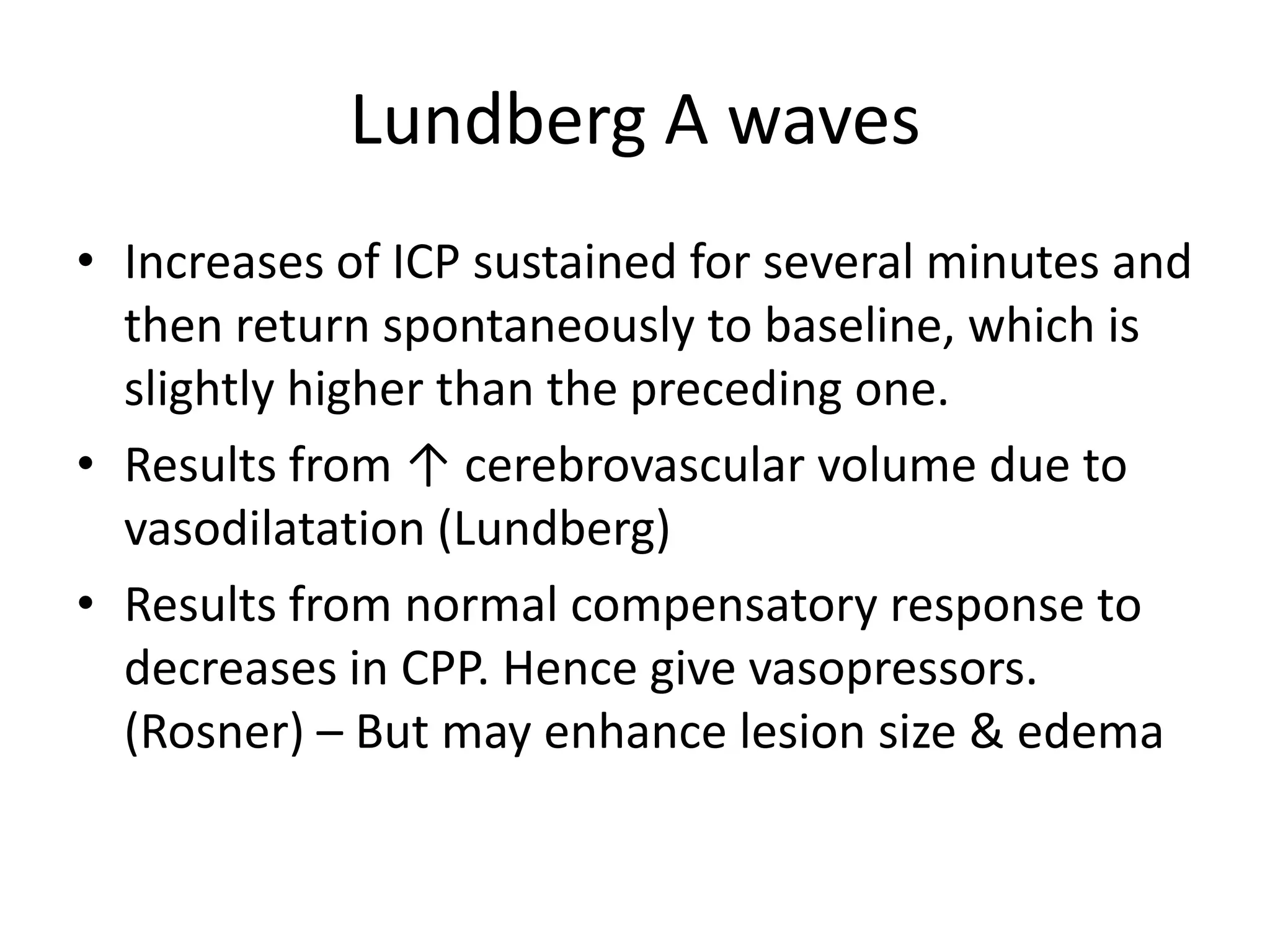
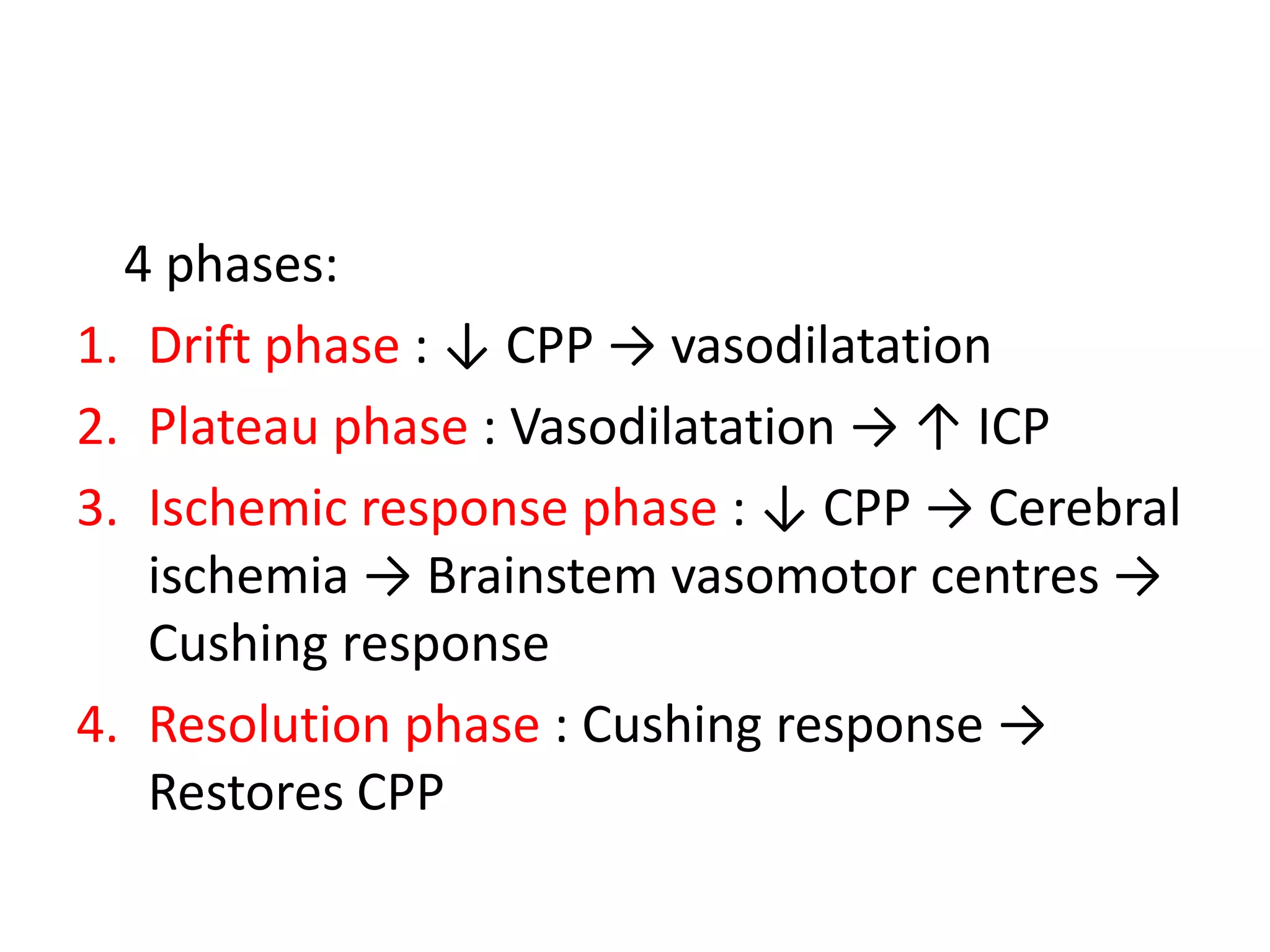
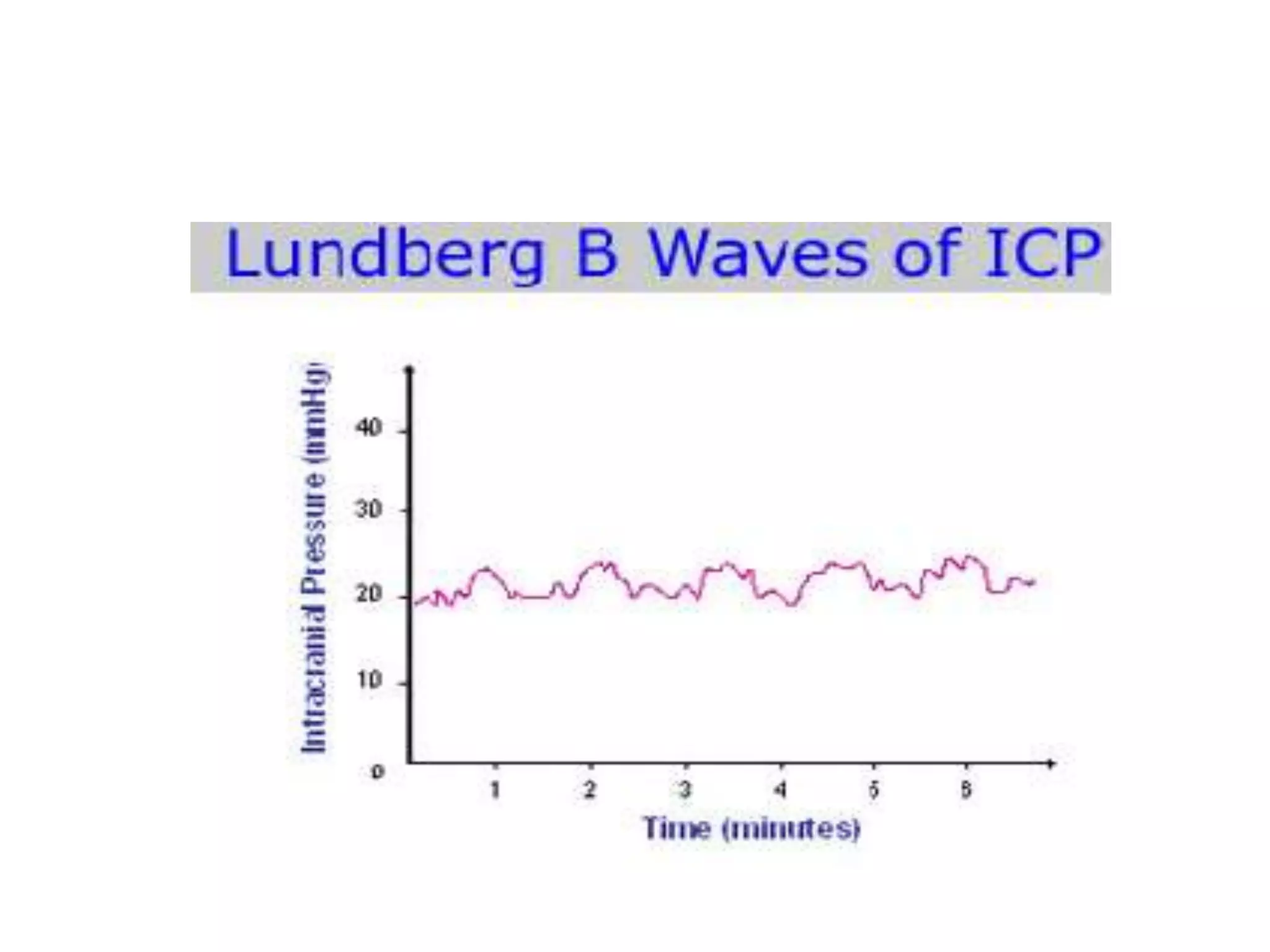
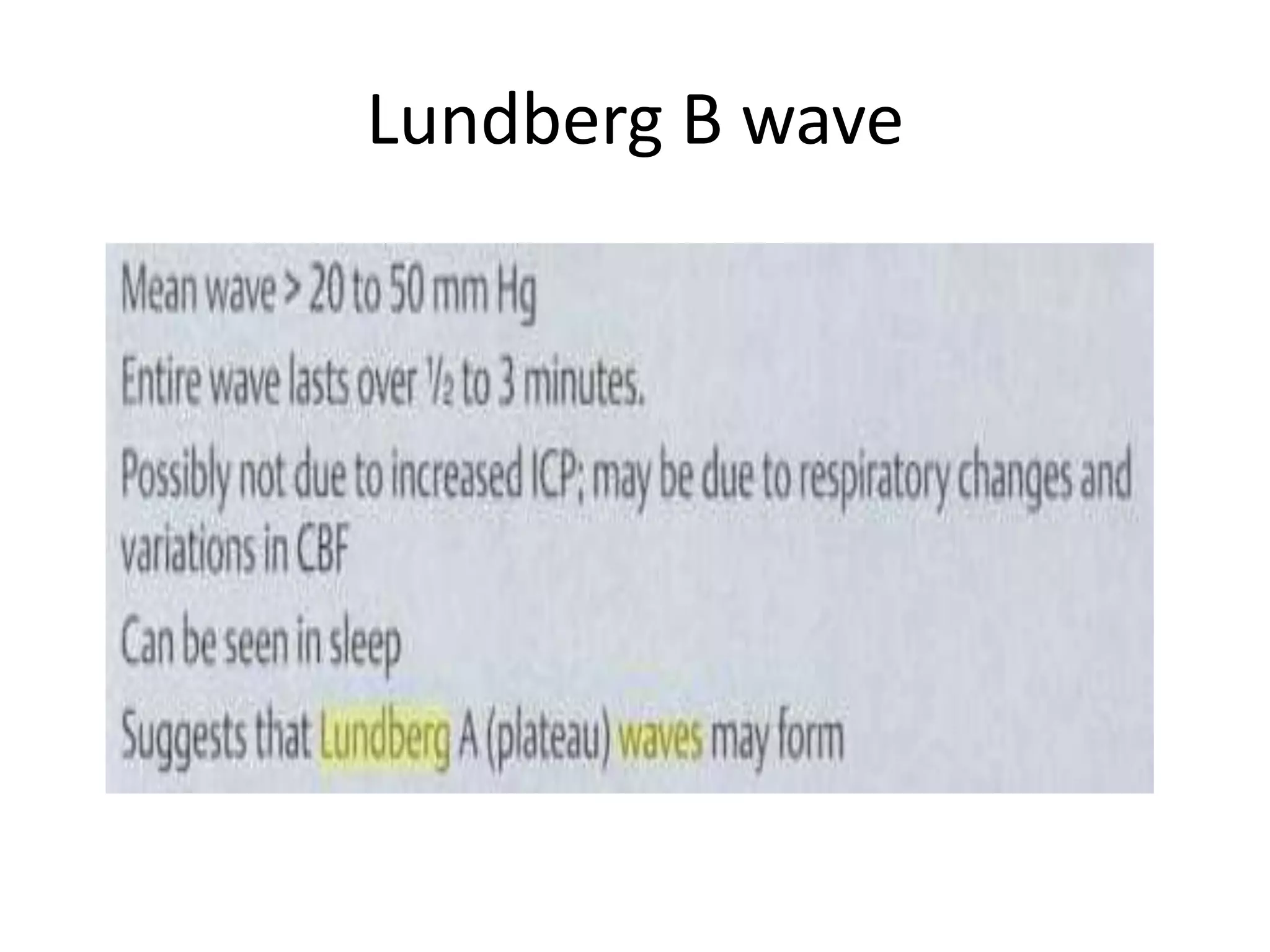
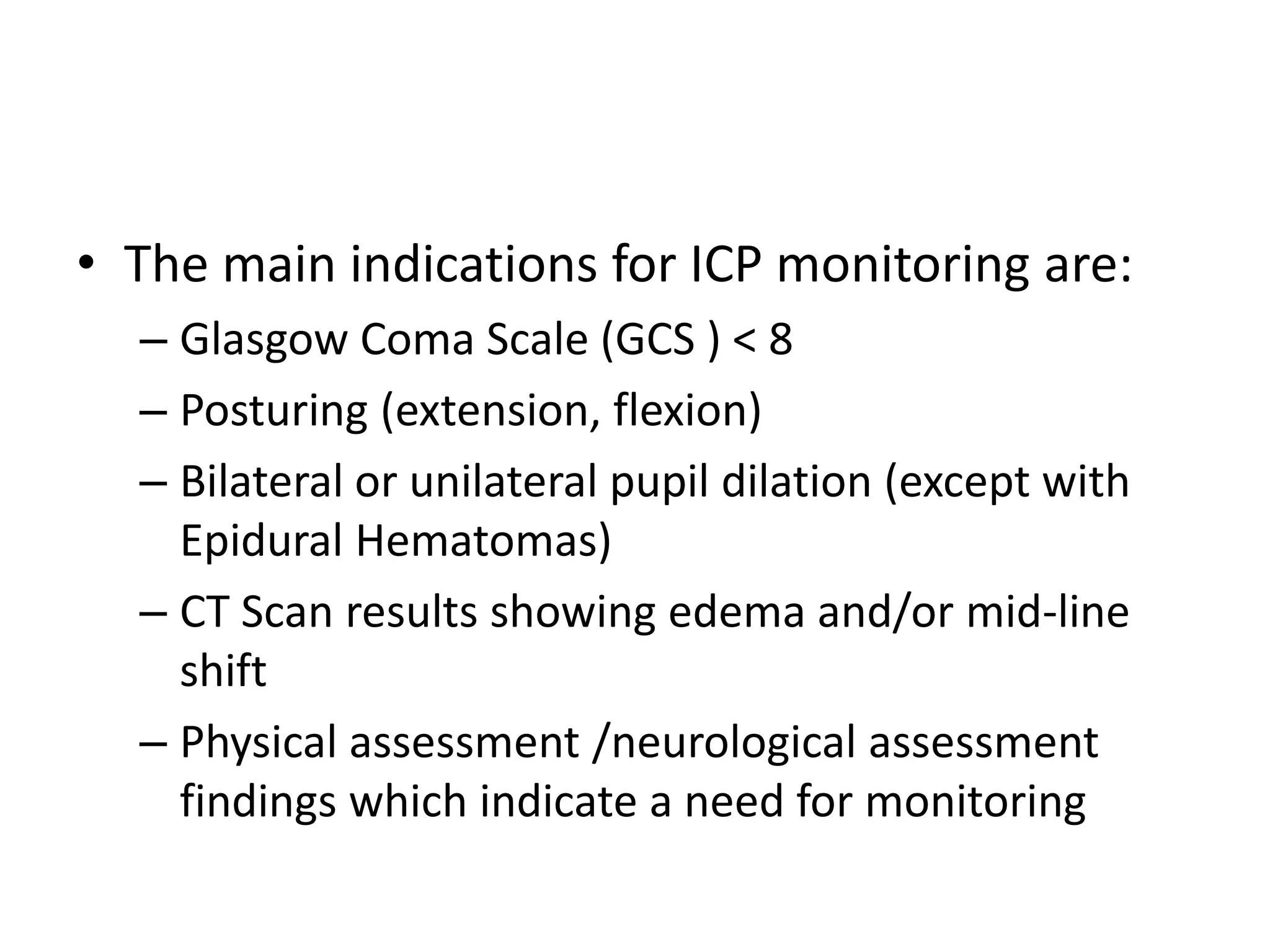
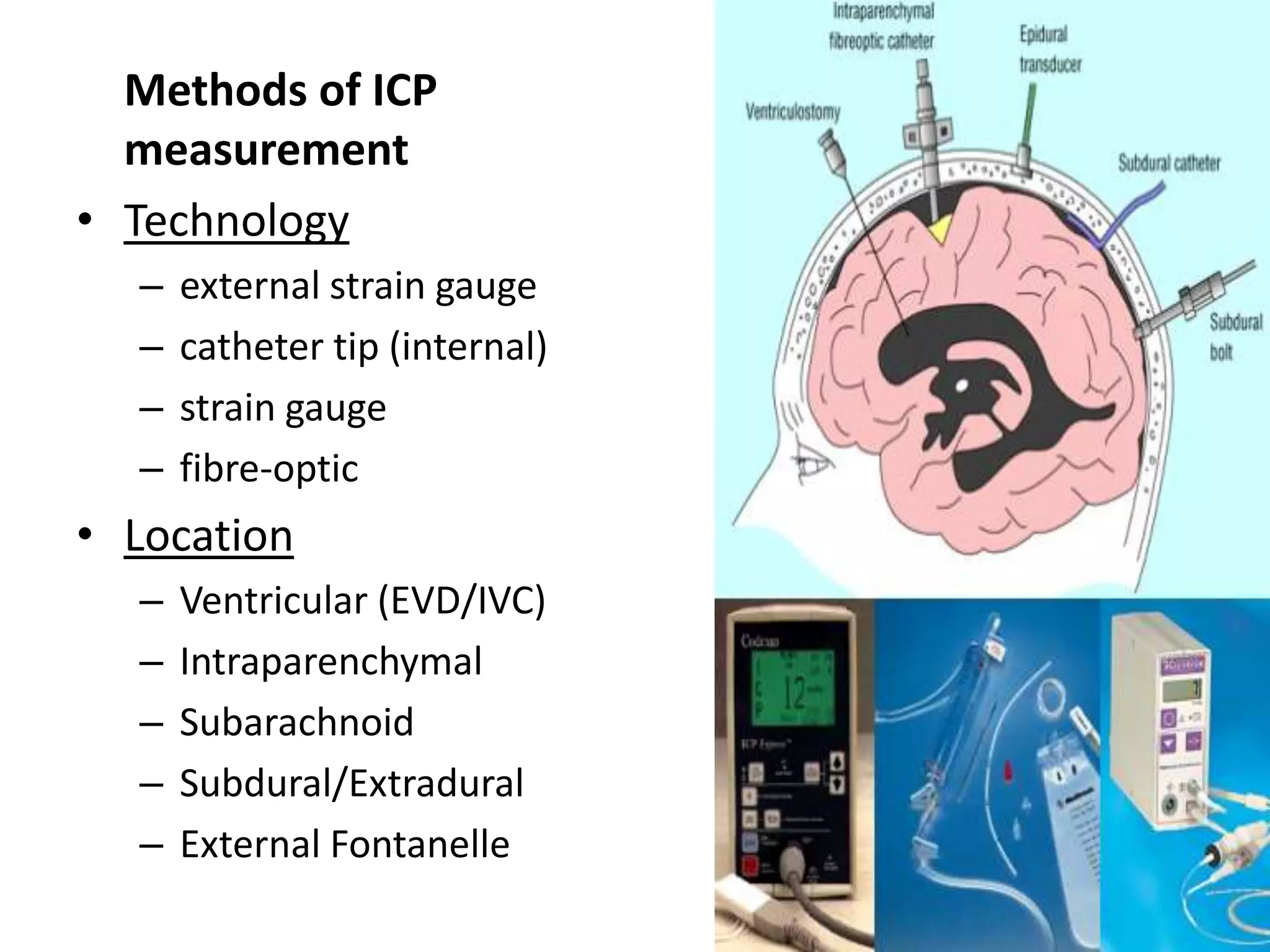
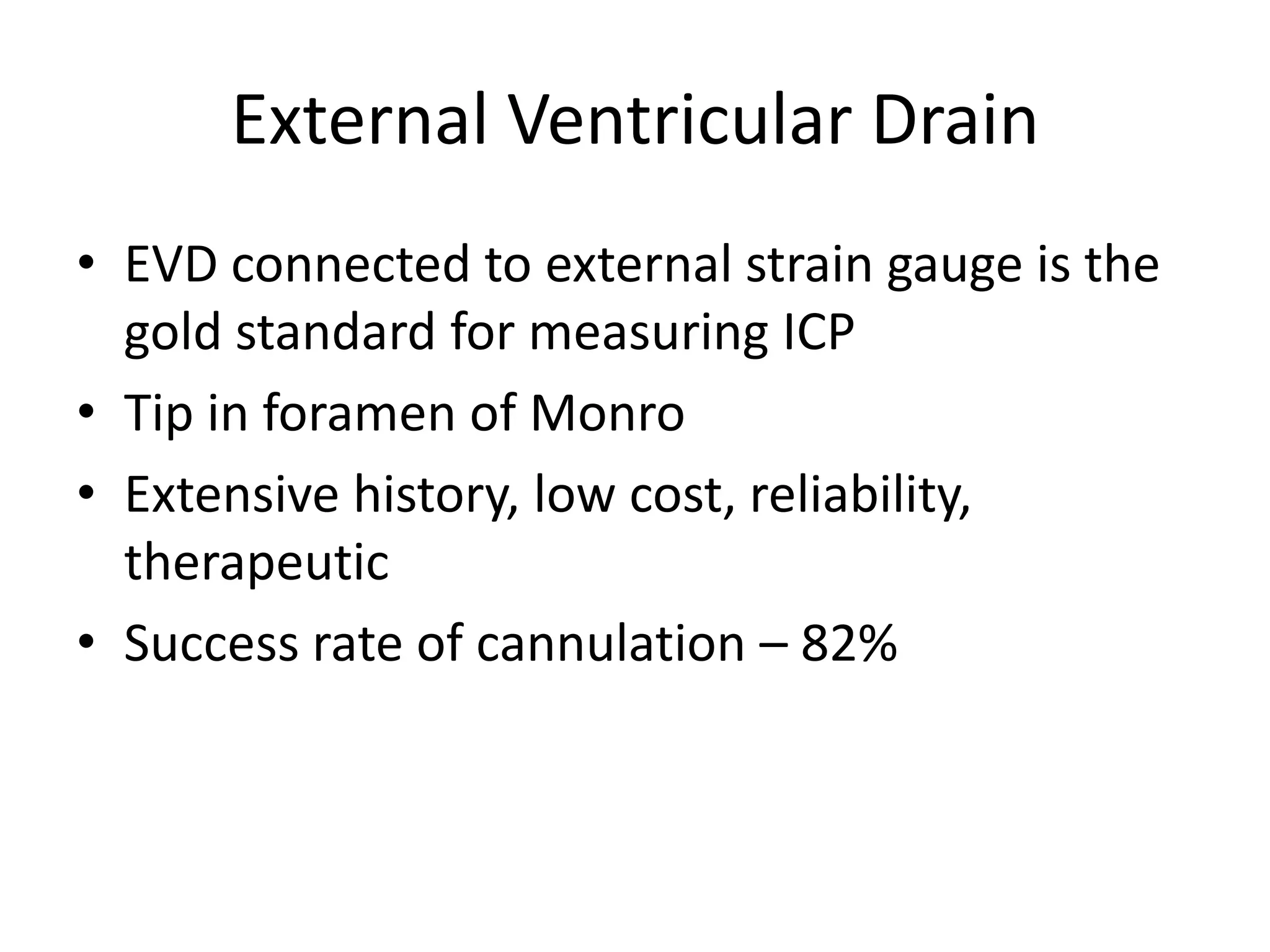
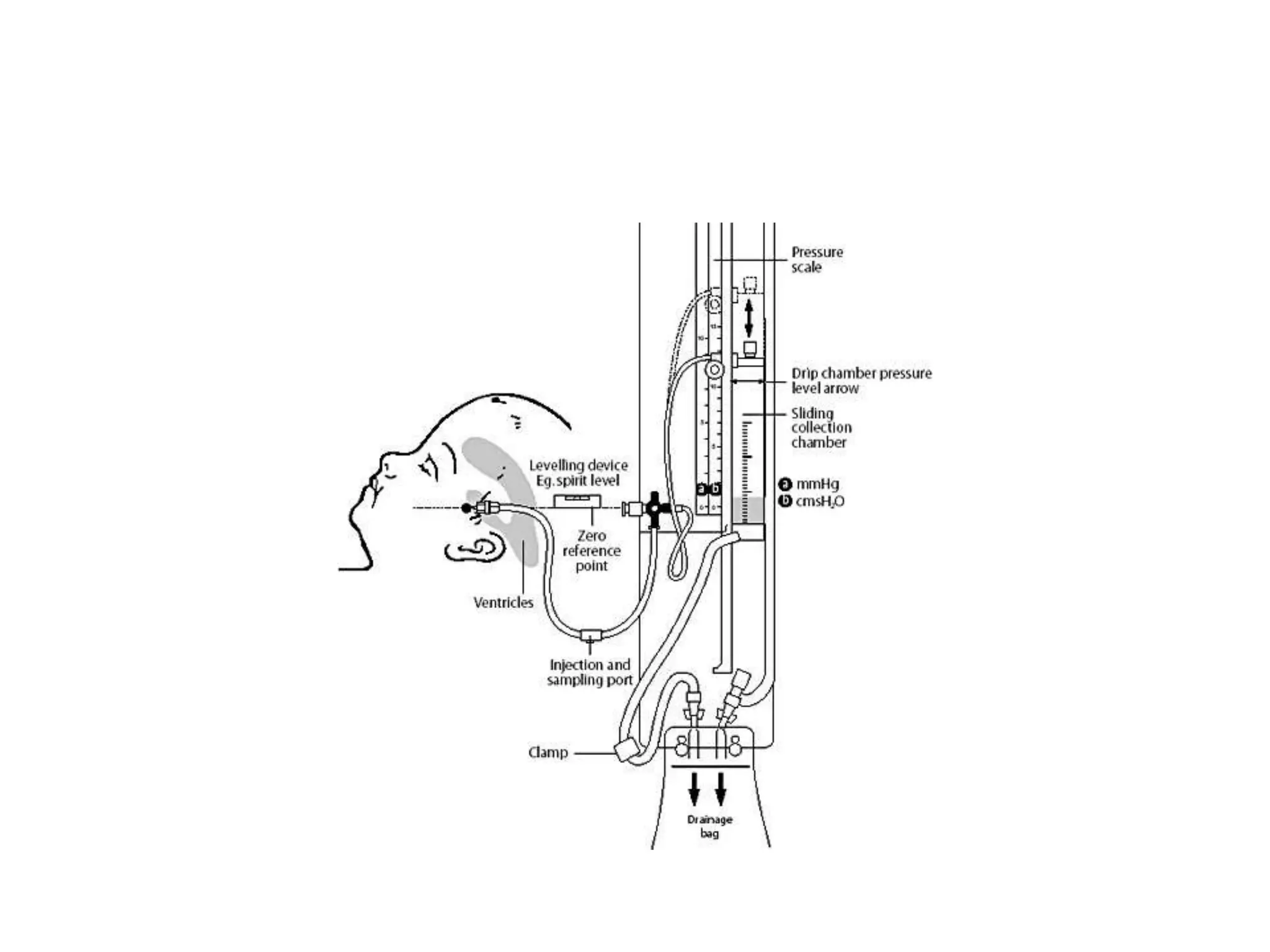
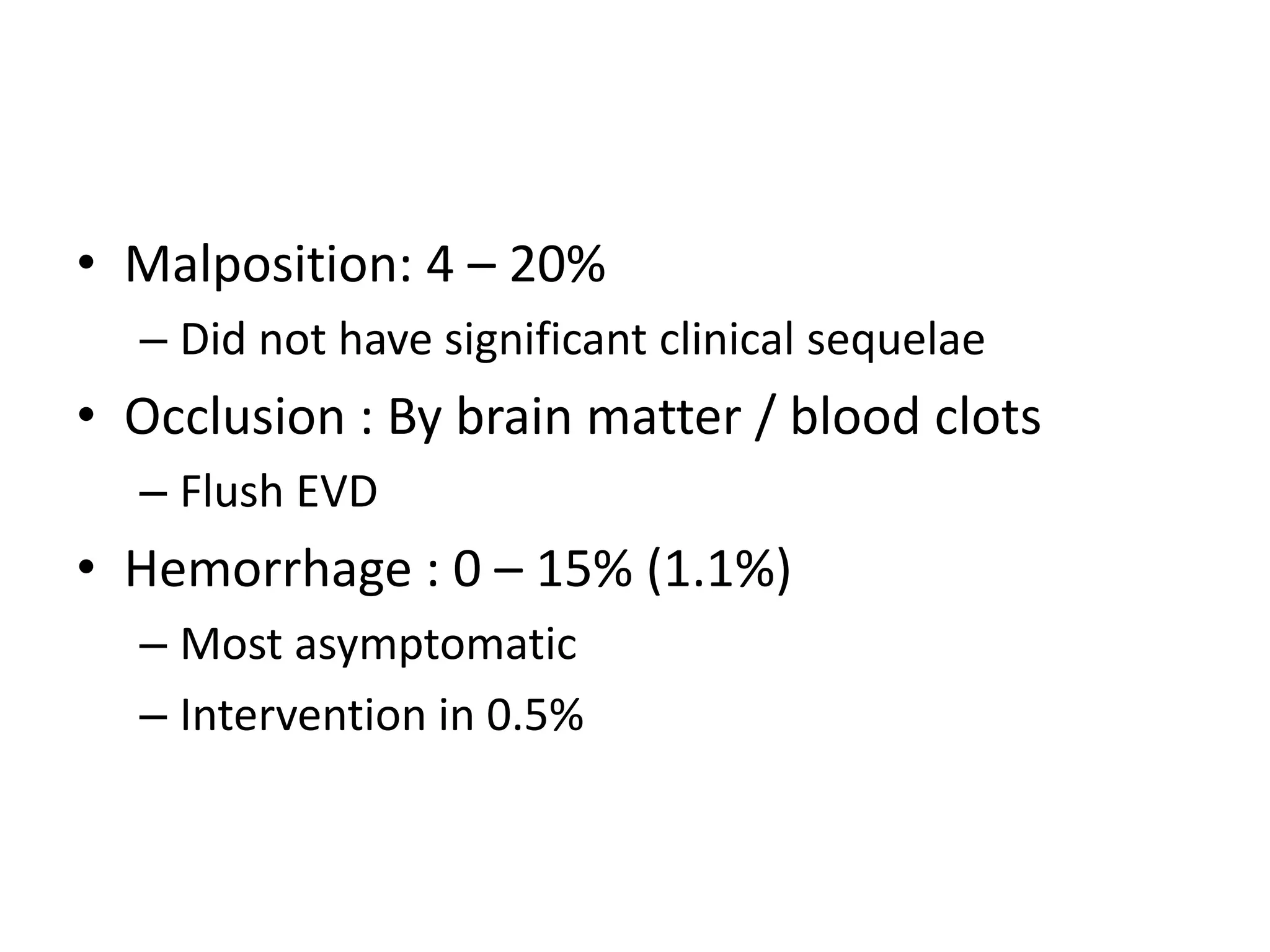
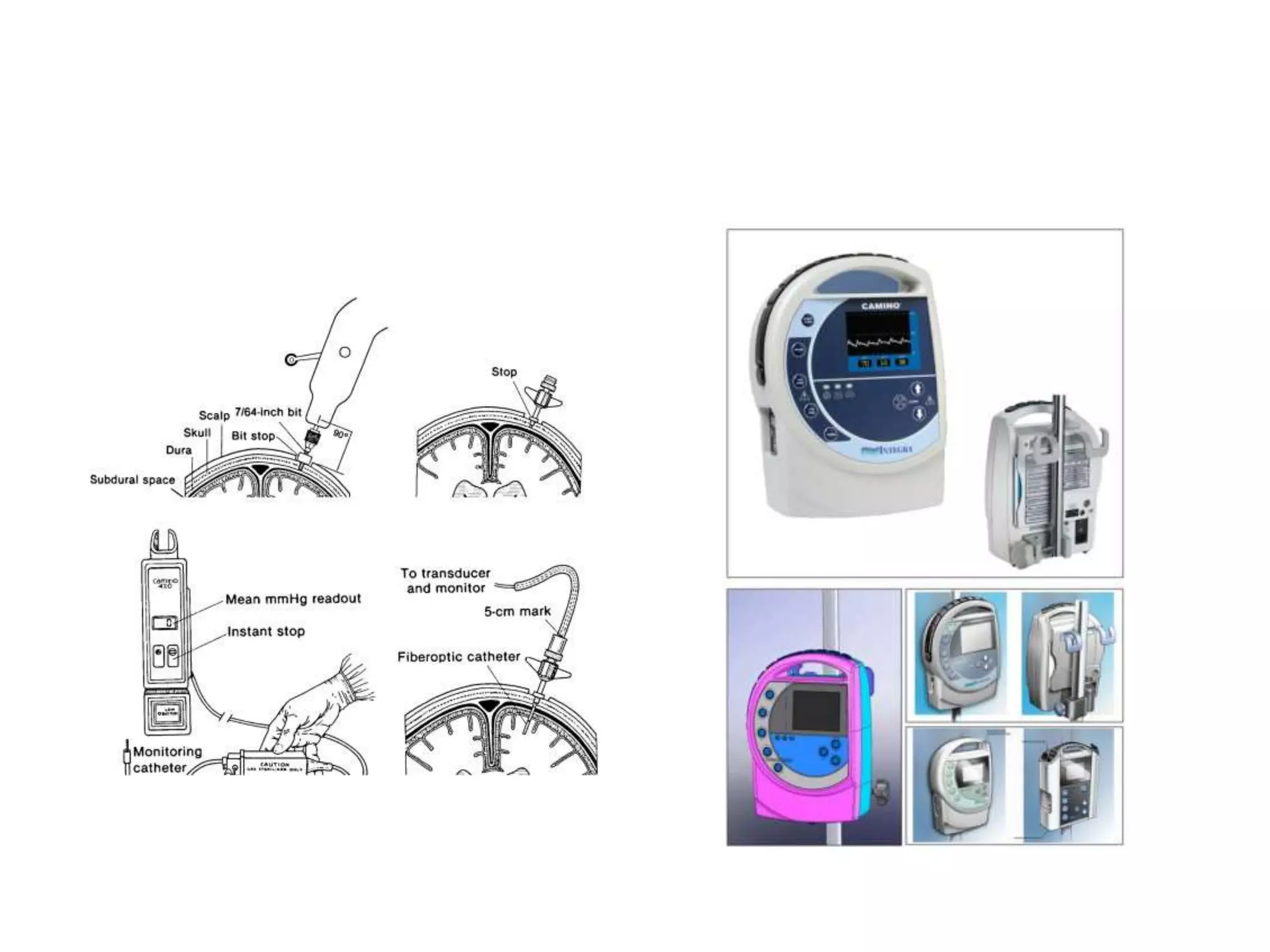
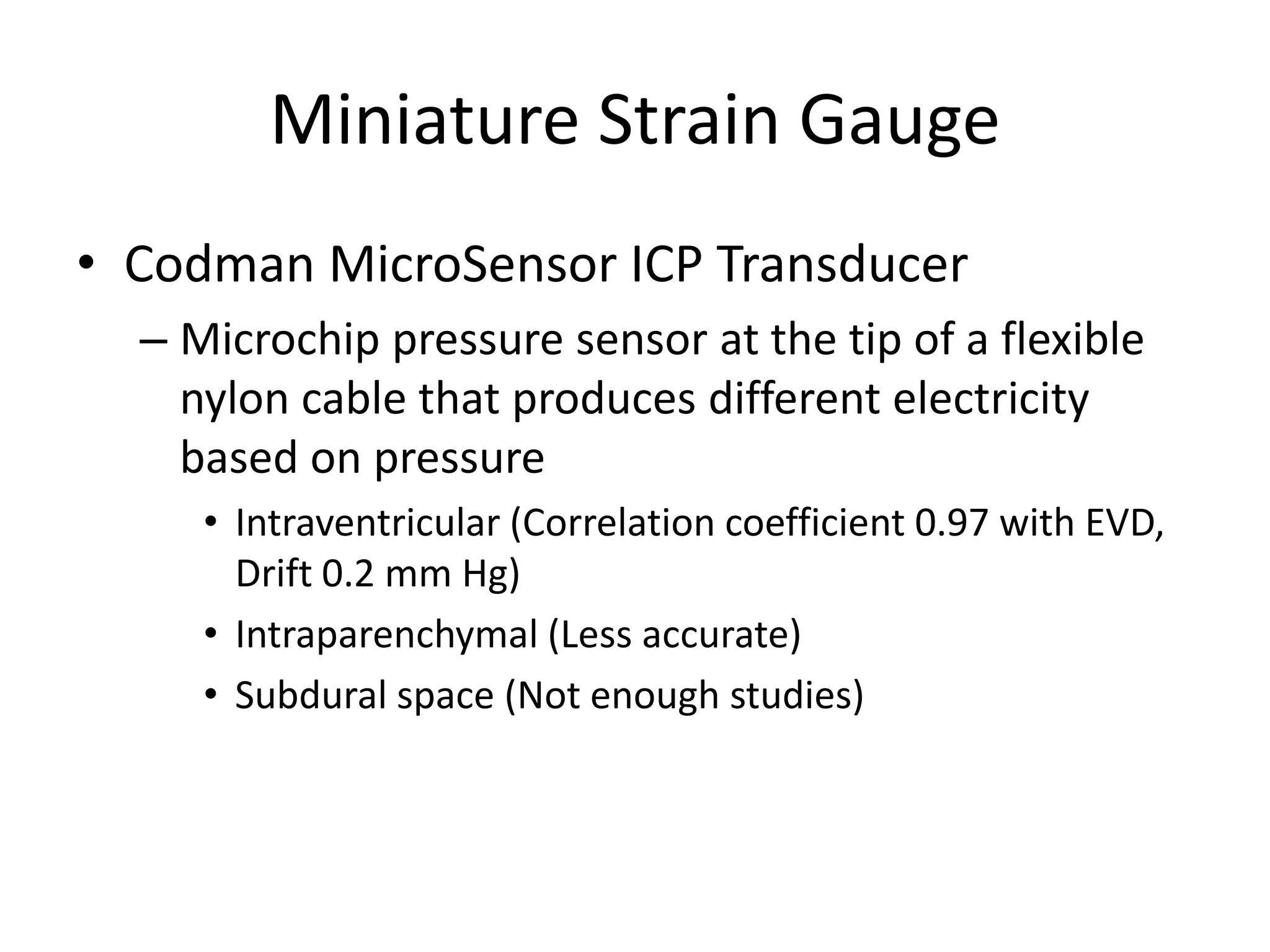
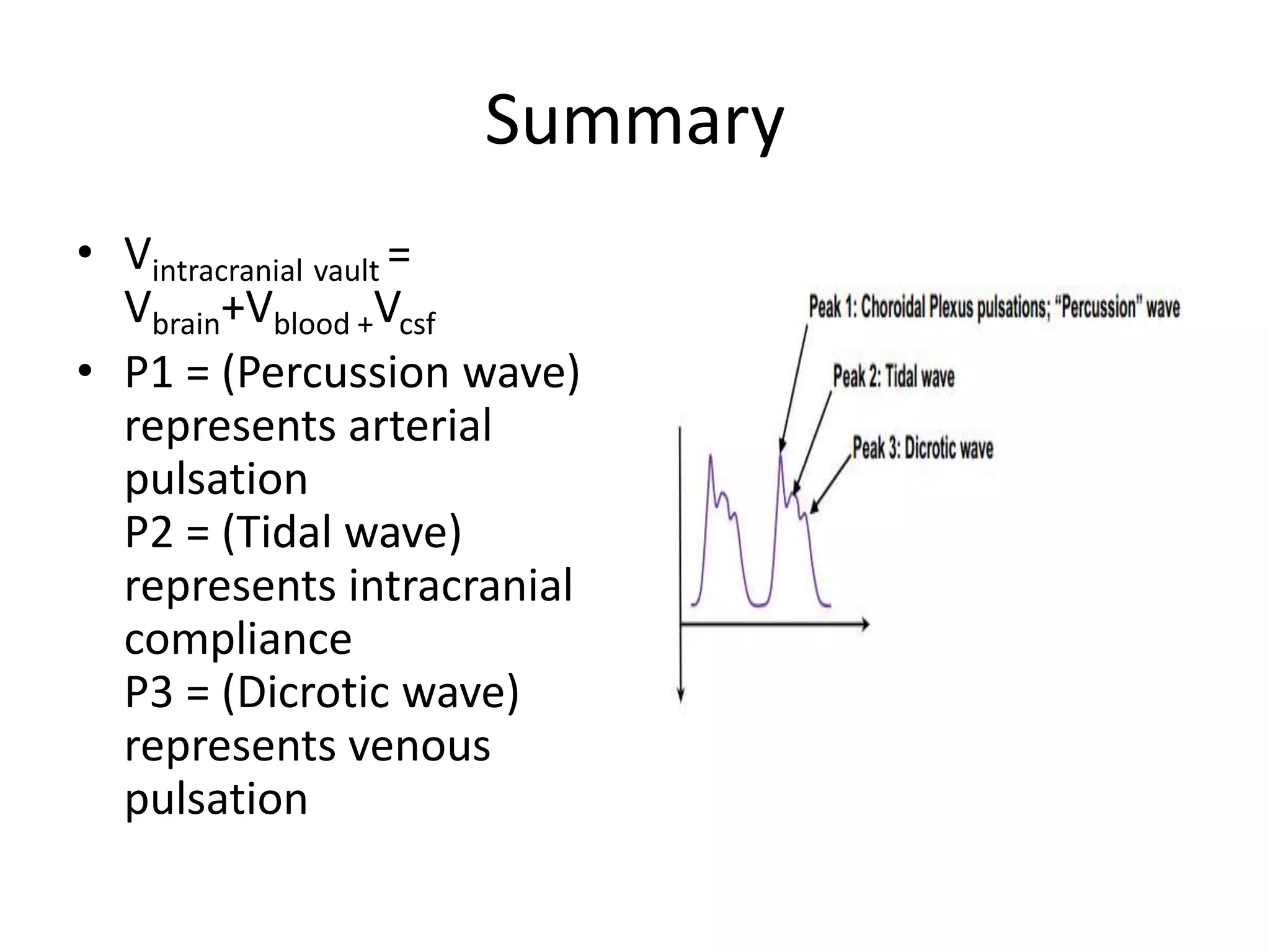
The document discusses intracranial pressure (ICP) waveforms and monitoring. It defines the components of the intracranial vault and describes the normal ICP waveform consisting of P1, P2, and P3 waves representing arterial pulsation, intracranial compliance, and venous pulsation, respectively. It also discusses Lundberg waves including A waves resulting from increased cerebrovascular volume due to vasodilation, B waves related to respiratory fluctuations in PaCO2, and C waves corresponding to Traube-Hering-Meyer fluctuations. The gold standard for ICP monitoring is external ventricular drainage connected to an external strain gauge, which allows CSF drainage but carries risks of infection and hemorrhage. Int