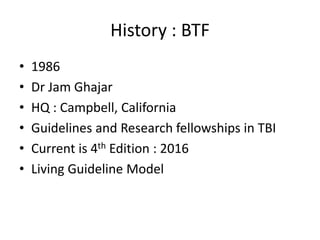
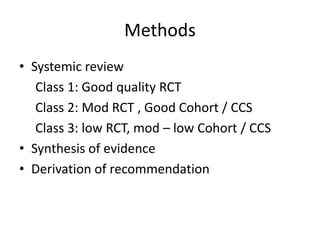
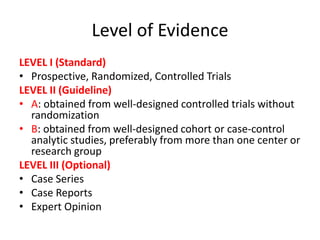
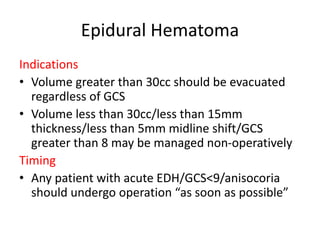
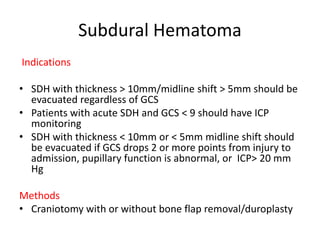
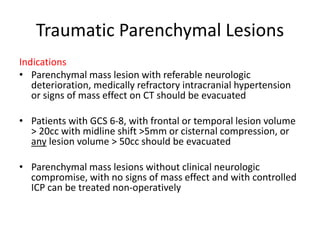
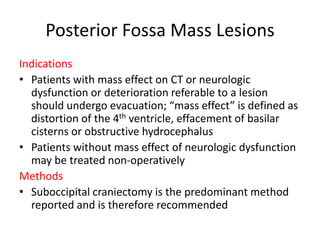
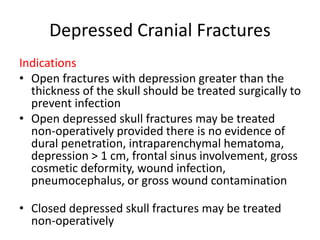
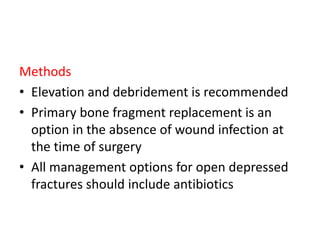
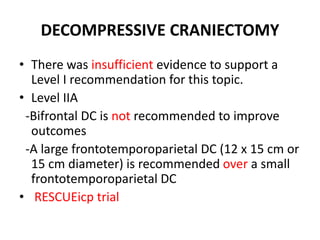
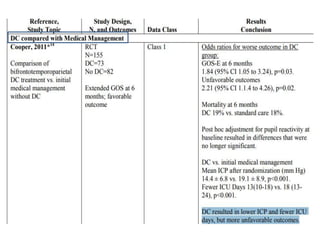
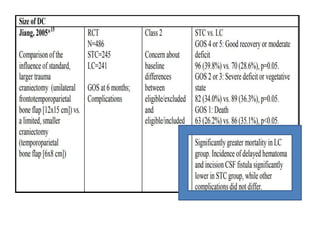
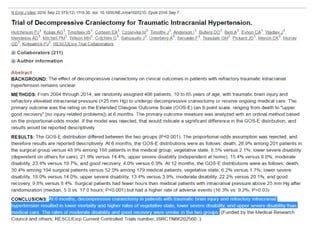
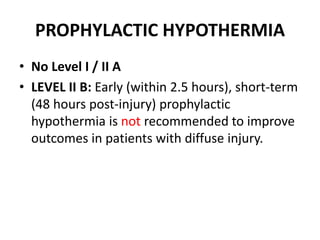
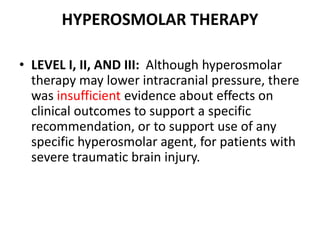
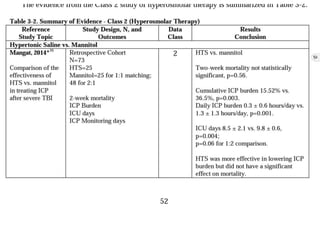
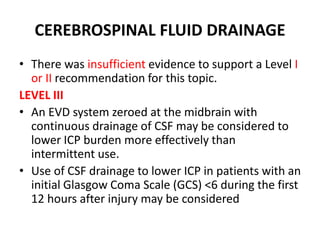
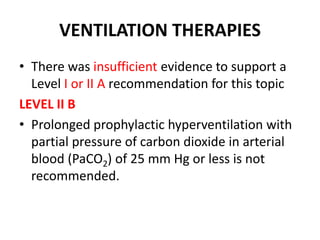
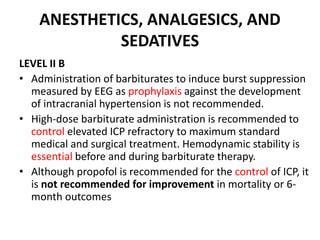
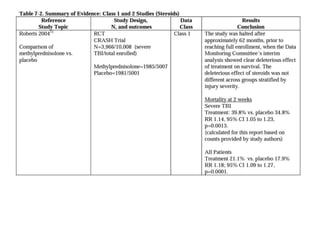
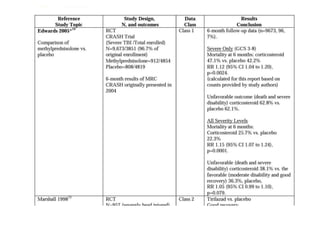
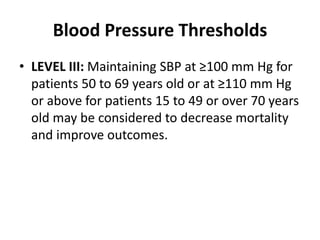
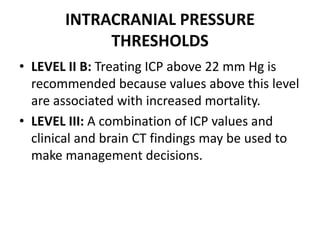
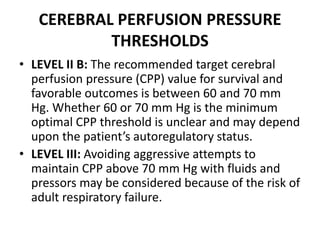
This document summarizes guidelines from the Brain Trauma Foundation (BTF) for the management of traumatic brain injury (TBI). It provides indications and recommendations for surgery on various brain injuries like epidural hematomas, subdural hematomas, and depressed skull fractures based on factors like volume and Glasgow Coma Scale. It also outlines Level I-III evidence for treatments, monitoring thresholds, and recommendations regarding intracranial pressure, cerebral perfusion pressure, seizures and other topics.