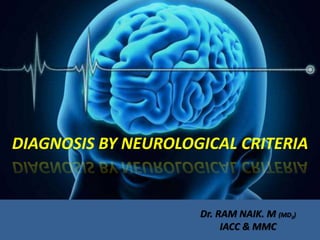
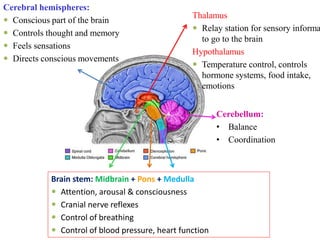
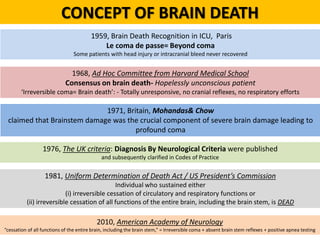
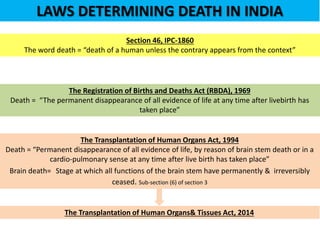
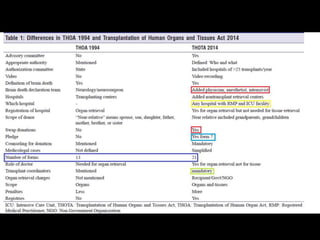
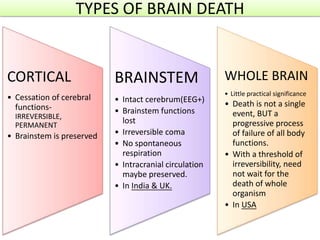
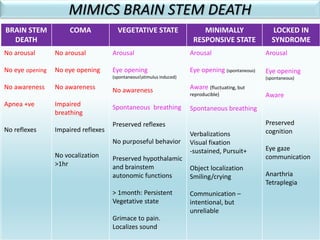
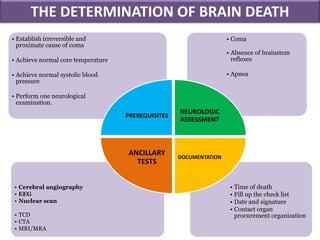
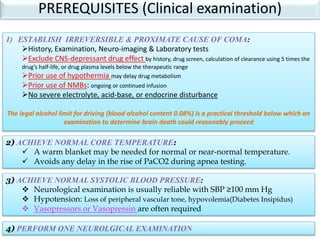
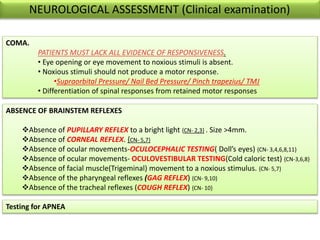
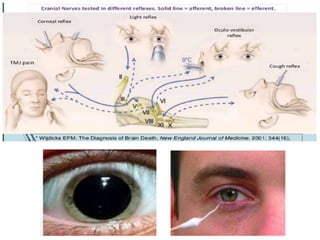
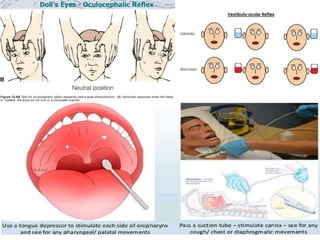
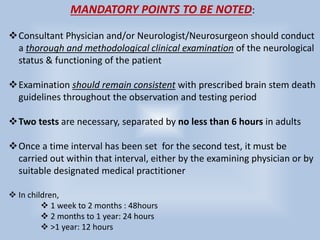
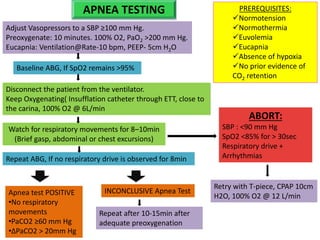
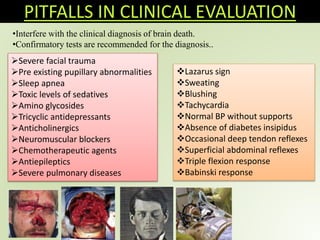
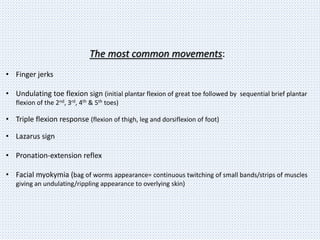
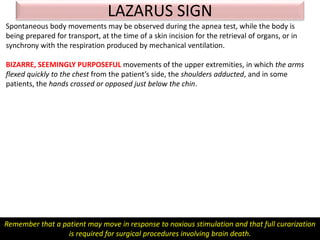
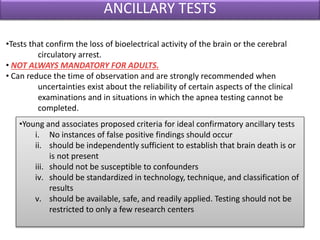
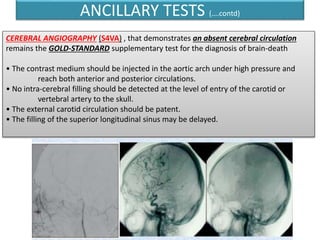
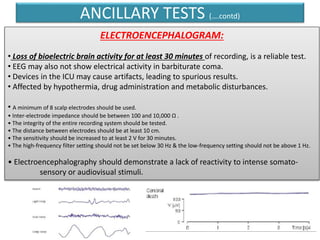
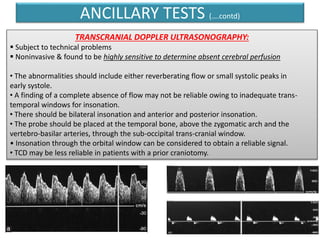
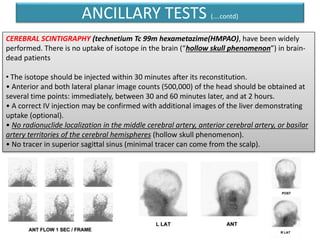
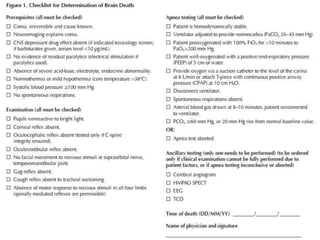
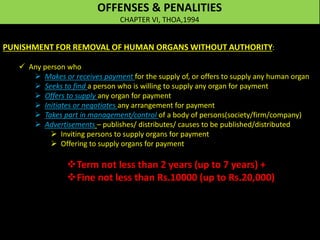
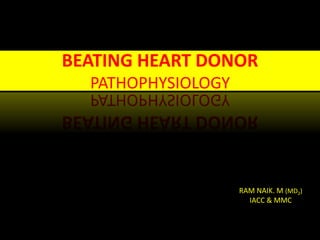
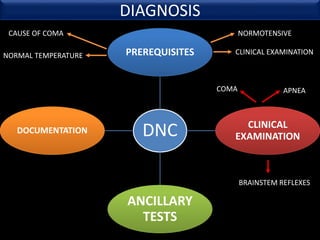
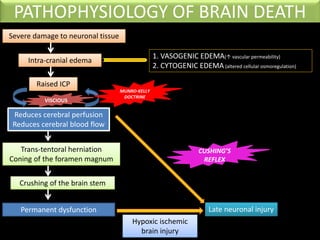
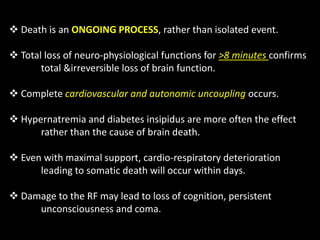
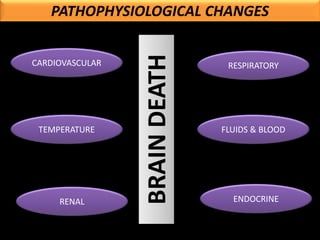
The document discusses the diagnosis of brain death through neurological criteria. It begins by describing the main parts of the brain and their functions. It then discusses the concepts, laws, and types of brain death in India. The key components of determining brain death are described, including establishing the cause of coma, achieving normal temperature and blood pressure, performing neurological examinations to check for absence of brainstem reflexes and response to stimuli, and conducting an apnea test. Potential mimics of brain death and pitfalls in the clinical evaluation are outlined. Confirmatory ancillary tests like cerebral angiography and EEG are also discussed.

![VENTILATORY SUPPORT
Lung protective mechanisms.
TV(6-9ml/kg) with optimal PEEP to maintain PaO2 > 70-80mm Hg
Optimal PEEP may reduce high FiO2 requirements. ( FiO2 to maintain SpO2 >90%)
Avoid PEEP > 15cm H2O
HOB 30-40 degrees
Tracheal cuff pressure 25cm H2O
Maintain normocarbia. (if not possible, moderate hypercarbia is permitted)
Recruitment maneuvers initially, repeat after apnea testing and tracheal suction.
If hyperventilation is employed, discontinue after diagnosis of Brain Death
Avoid administration of excess IVF. (Consider Diuretics, if marked fluid overload)
ABG every 4 hours, After 30min of change in settings
Paw< 40 m H2O
Pplat <35 cm H2O
FiO2- [ SpO2>92% and PaO2 > 70-80mm Hg]
Rate- To maintain normocarbia and pH
Auto PEEP < 5 cm H2O
TV- 6-9ml/kg](https://image.slidesharecdn.com/braindeath-201001014732/85/Brain-death-61-320.jpg)