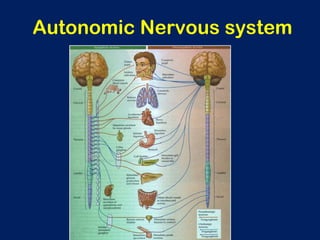
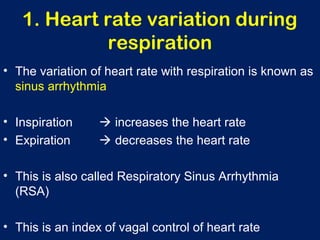
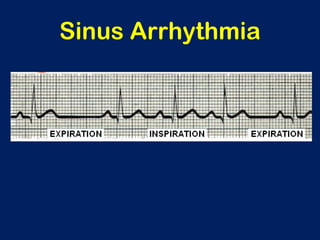
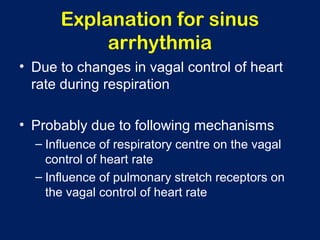
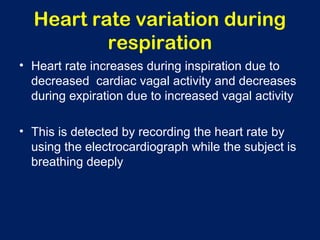
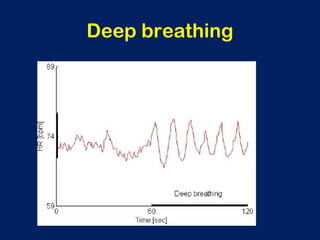
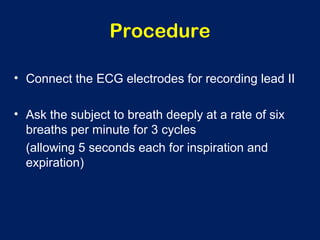
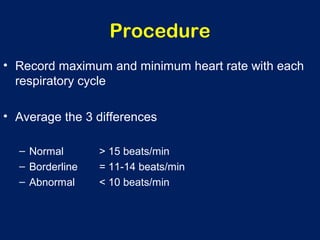
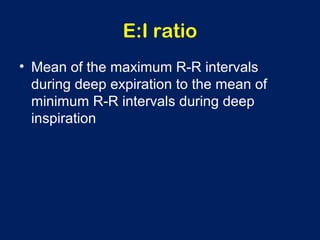
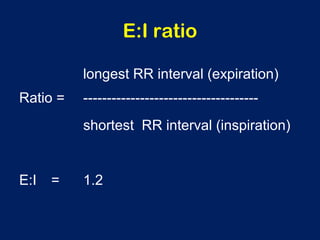
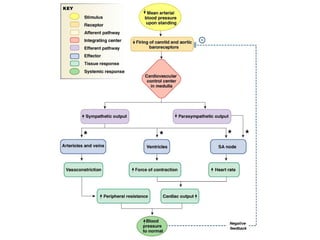
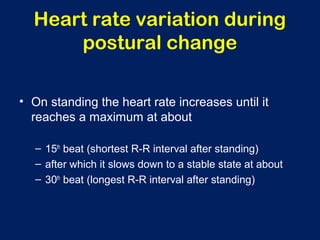
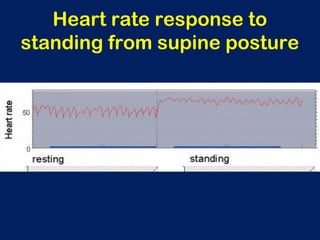
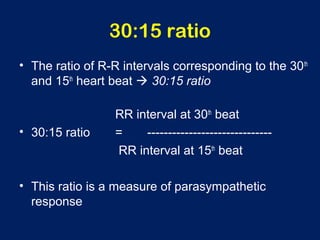
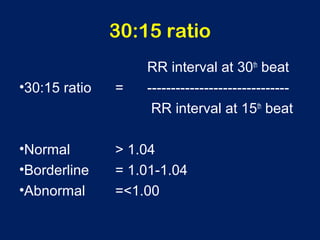
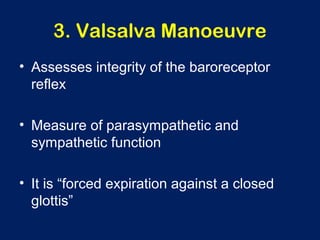
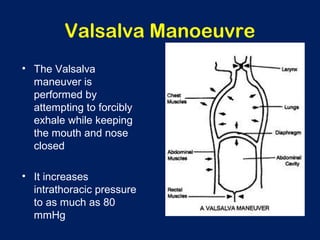
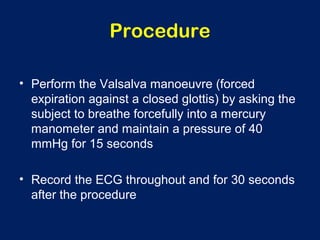
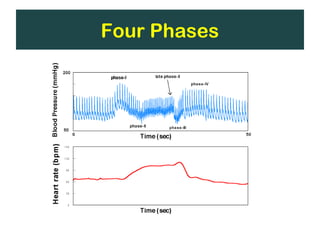
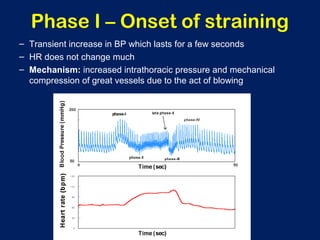
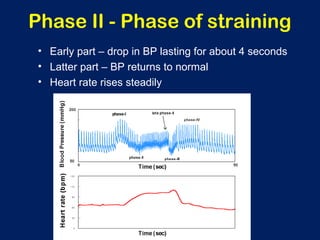
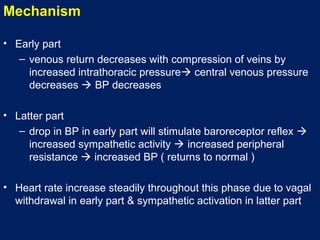
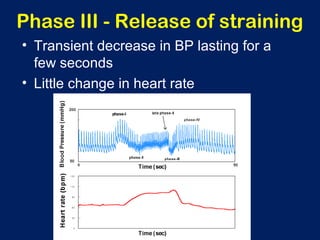
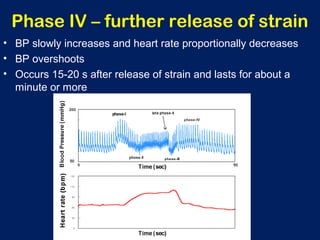
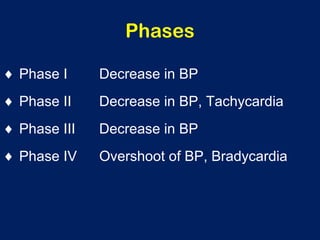
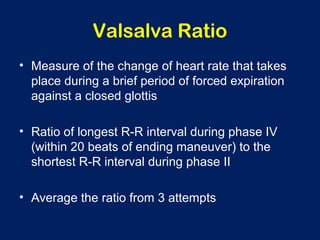
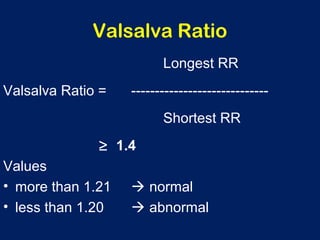
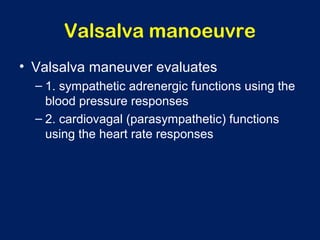
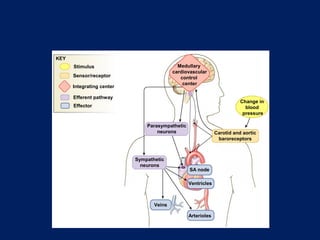
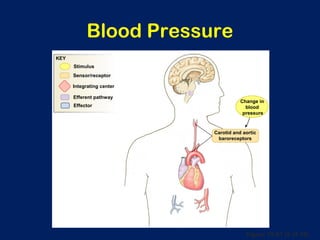
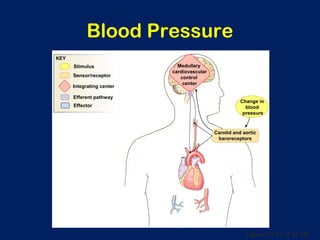
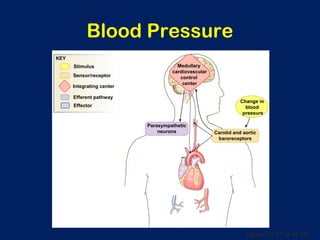
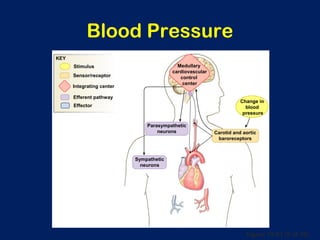
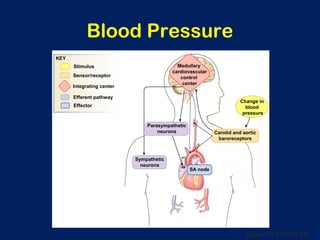
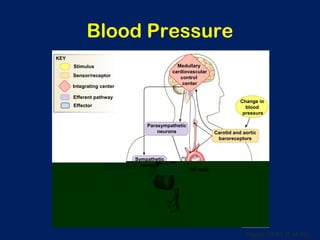
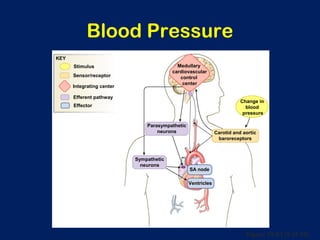
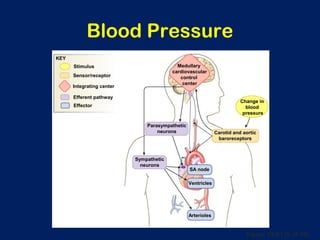
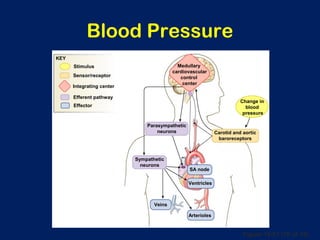
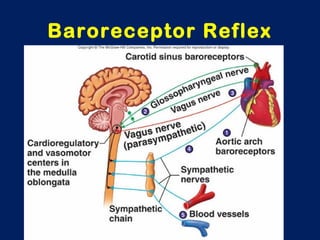
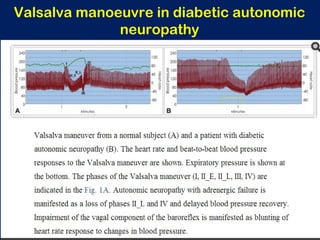
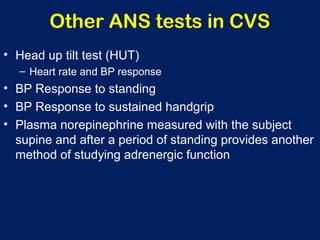
The document describes four autonomic function tests related to the cardiovascular system: 1) Heart rate variation during respiration measures vagal control of heart rate, 2) Heart rate variation during postural change assesses parasympathetic response, 3) The Valsalva maneuver evaluates sympathetic and parasympathetic function by measuring blood pressure and heart rate responses to forced exhalation, 4) The cold pressor test increases blood pressure by submerging a hand in ice water to stimulate the sympathetic nervous system. These tests are used to evaluate autonomic nervous system integrity.