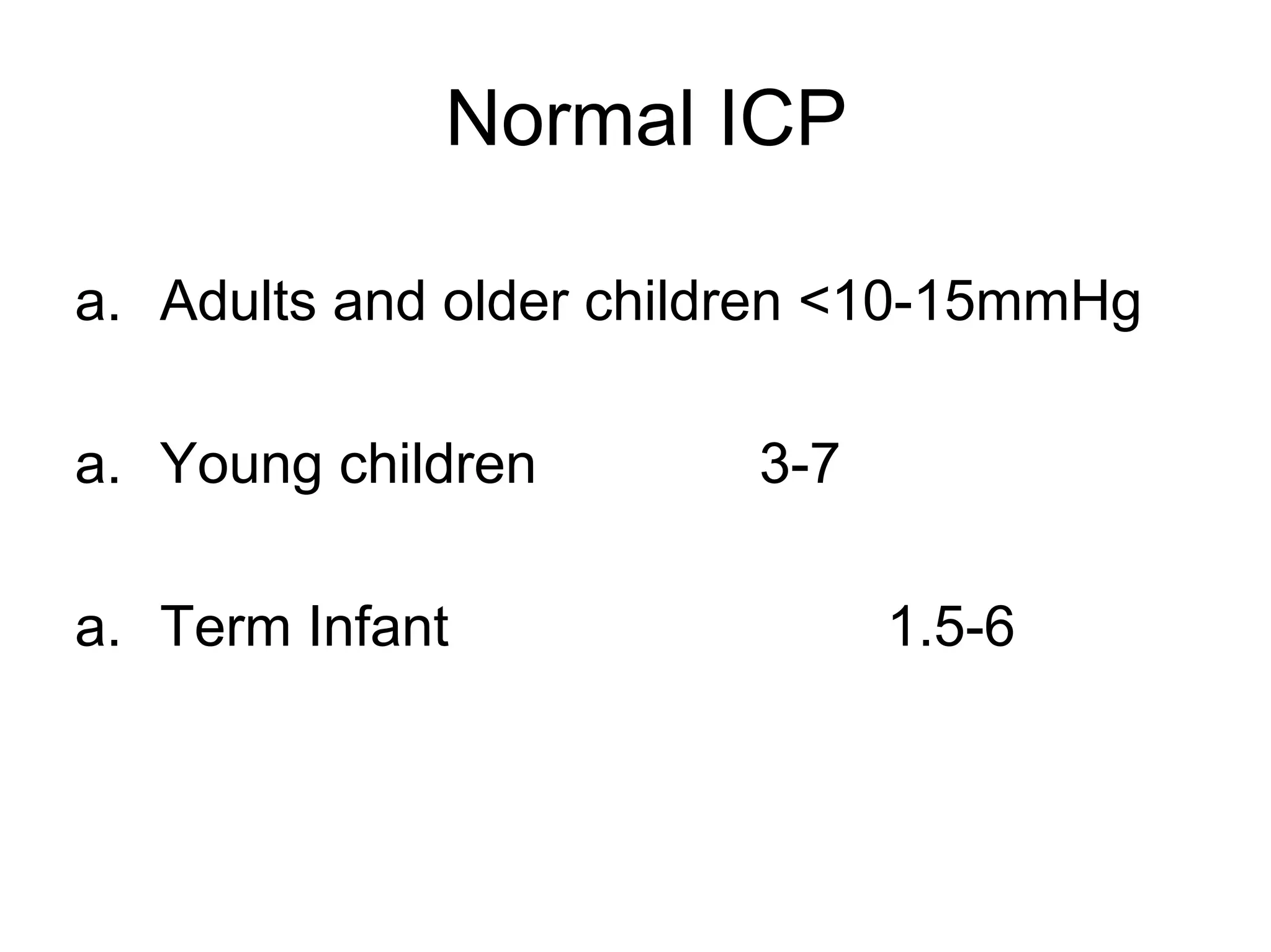
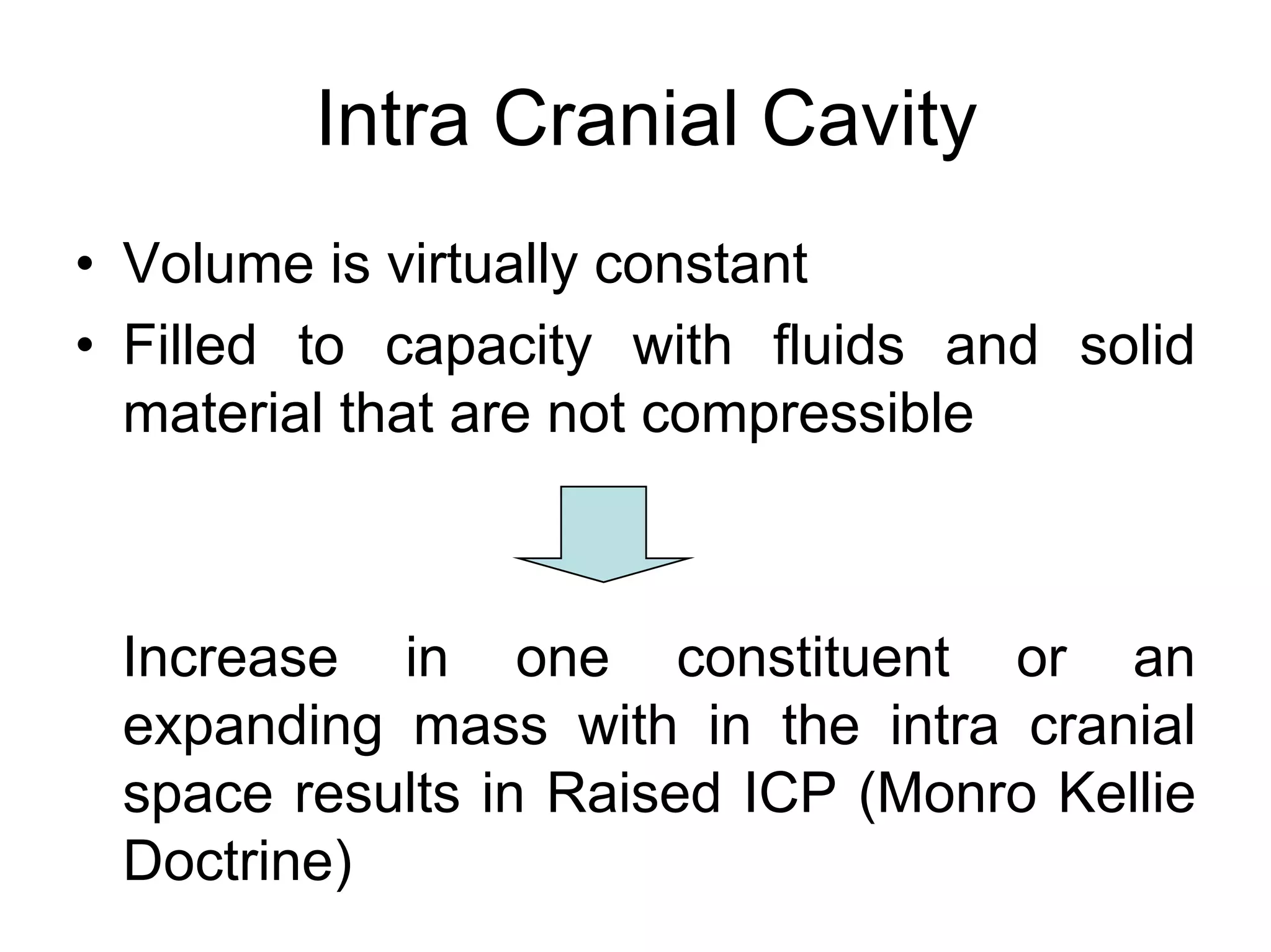
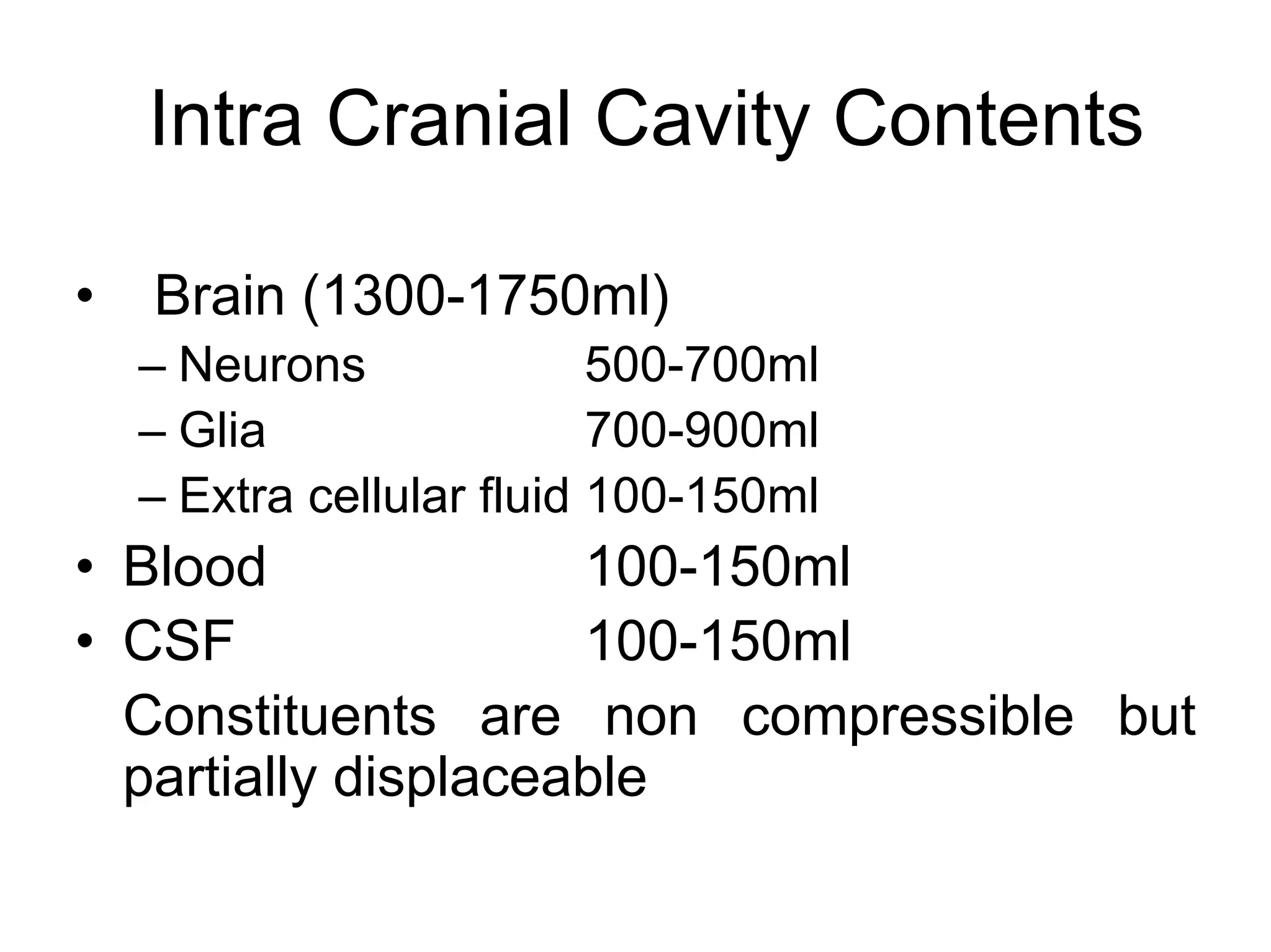
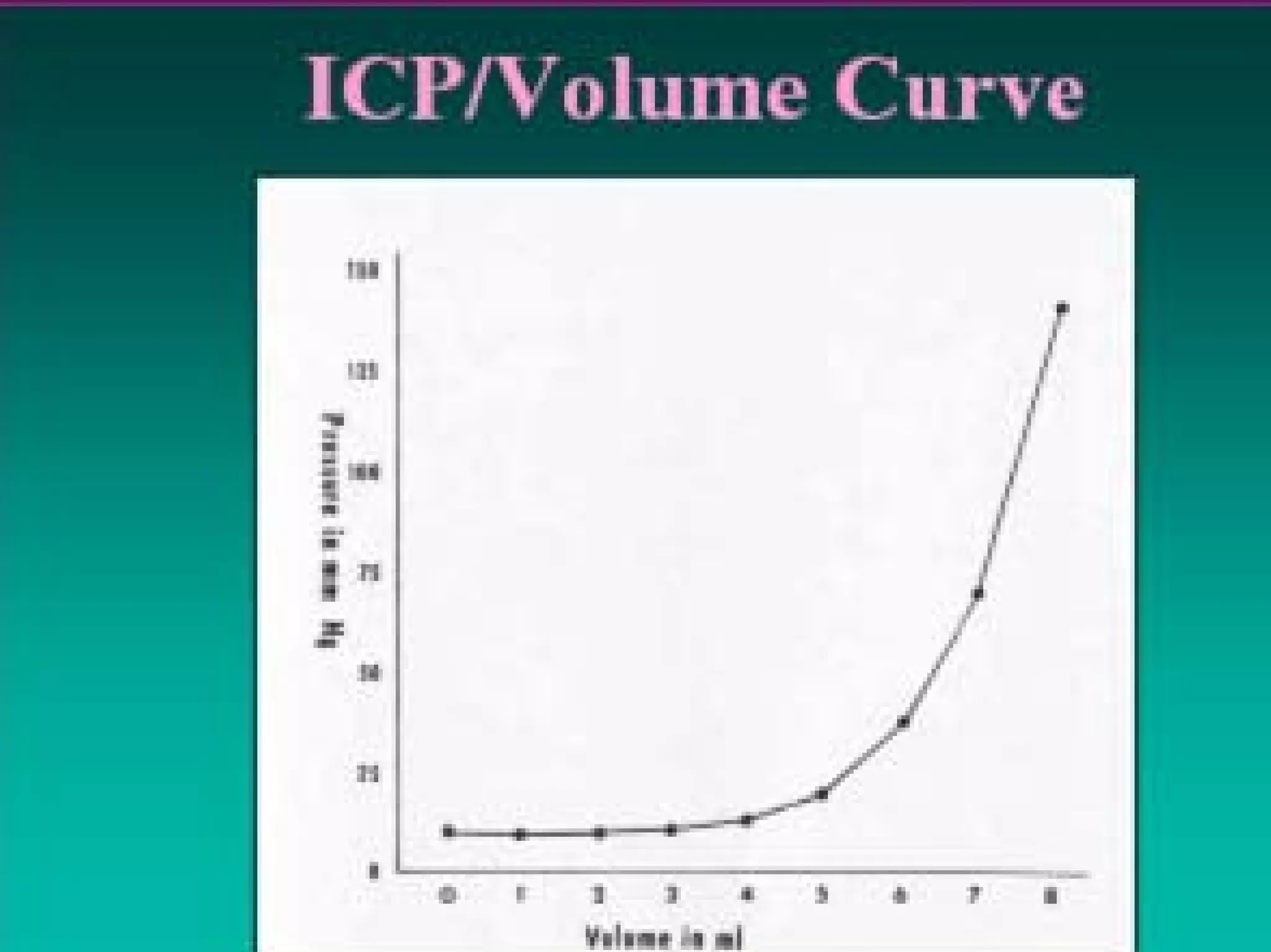
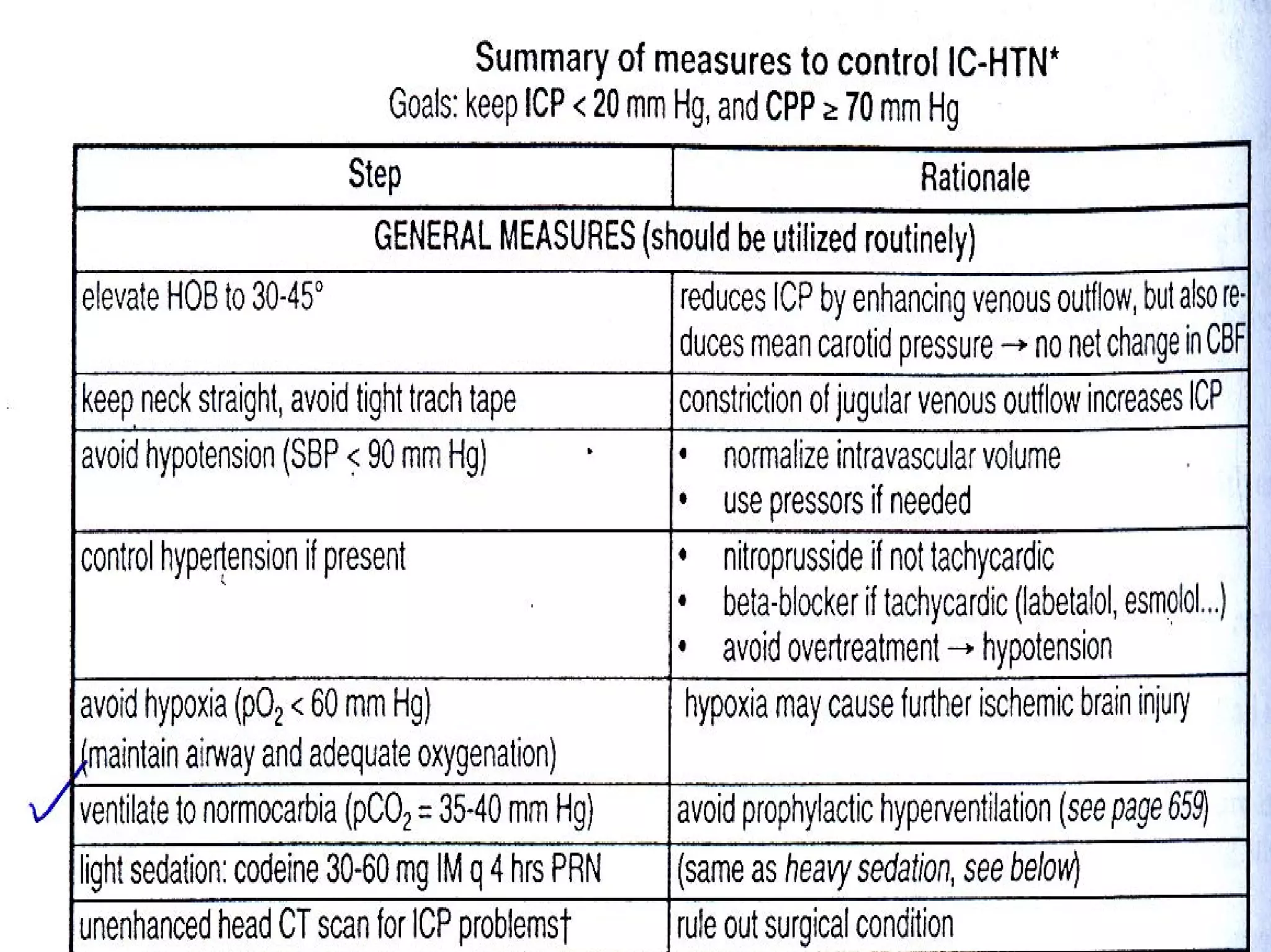
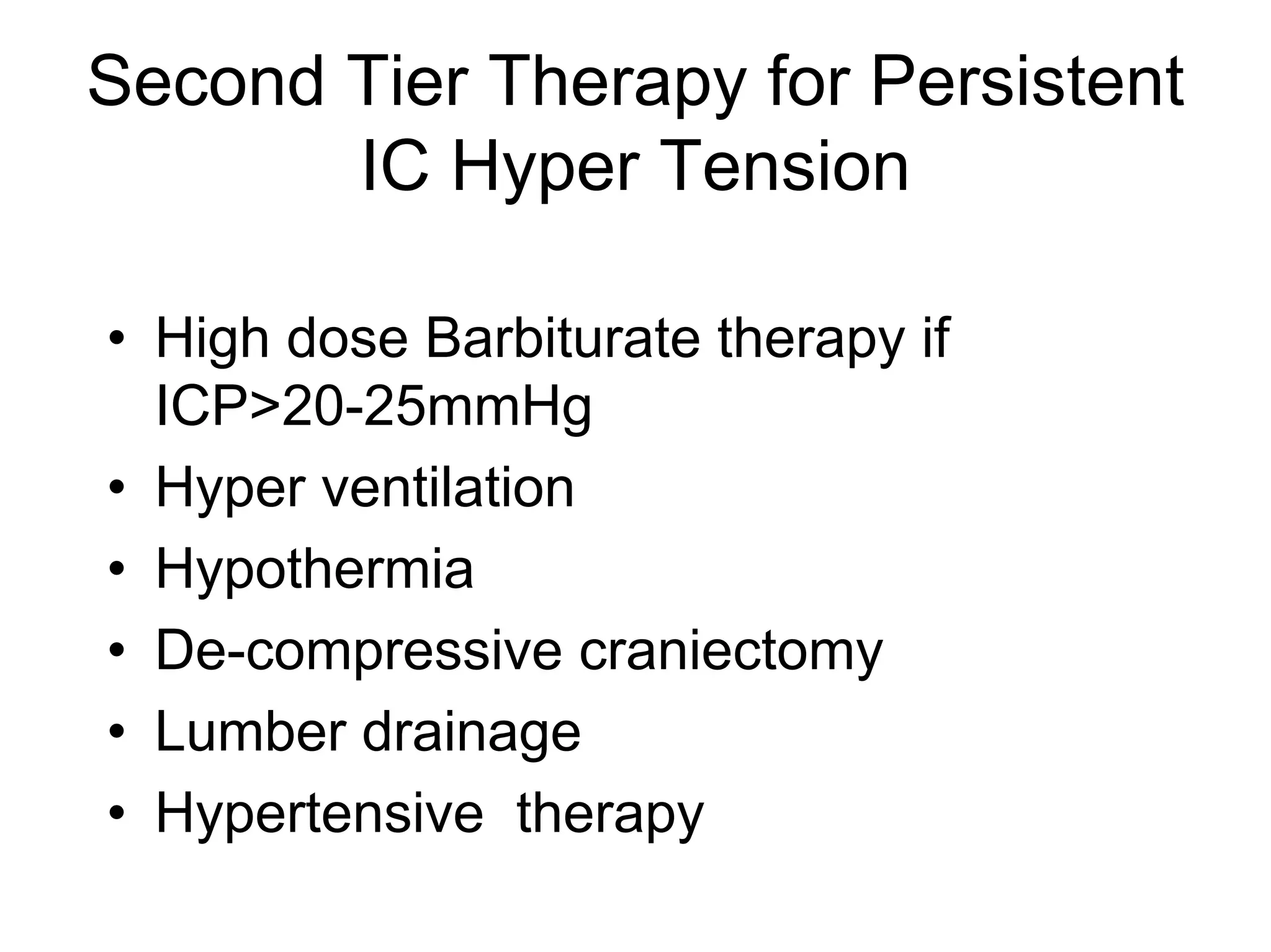
This document discusses monitoring and management of raised intracranial pressure. It begins by defining normal intracranial pressure ranges and describing the components of the intracranial cavity. Clinical signs of raised ICP are then outlined, followed by common causes and mechanisms. Monitoring of ICP is described including indications, contraindications and different monitoring device types. Treatment measures to lower ICP are then covered at both general and specific levels, including surgical intervention, ventilation management, barbiturate therapy, and decompressive craniectomy.