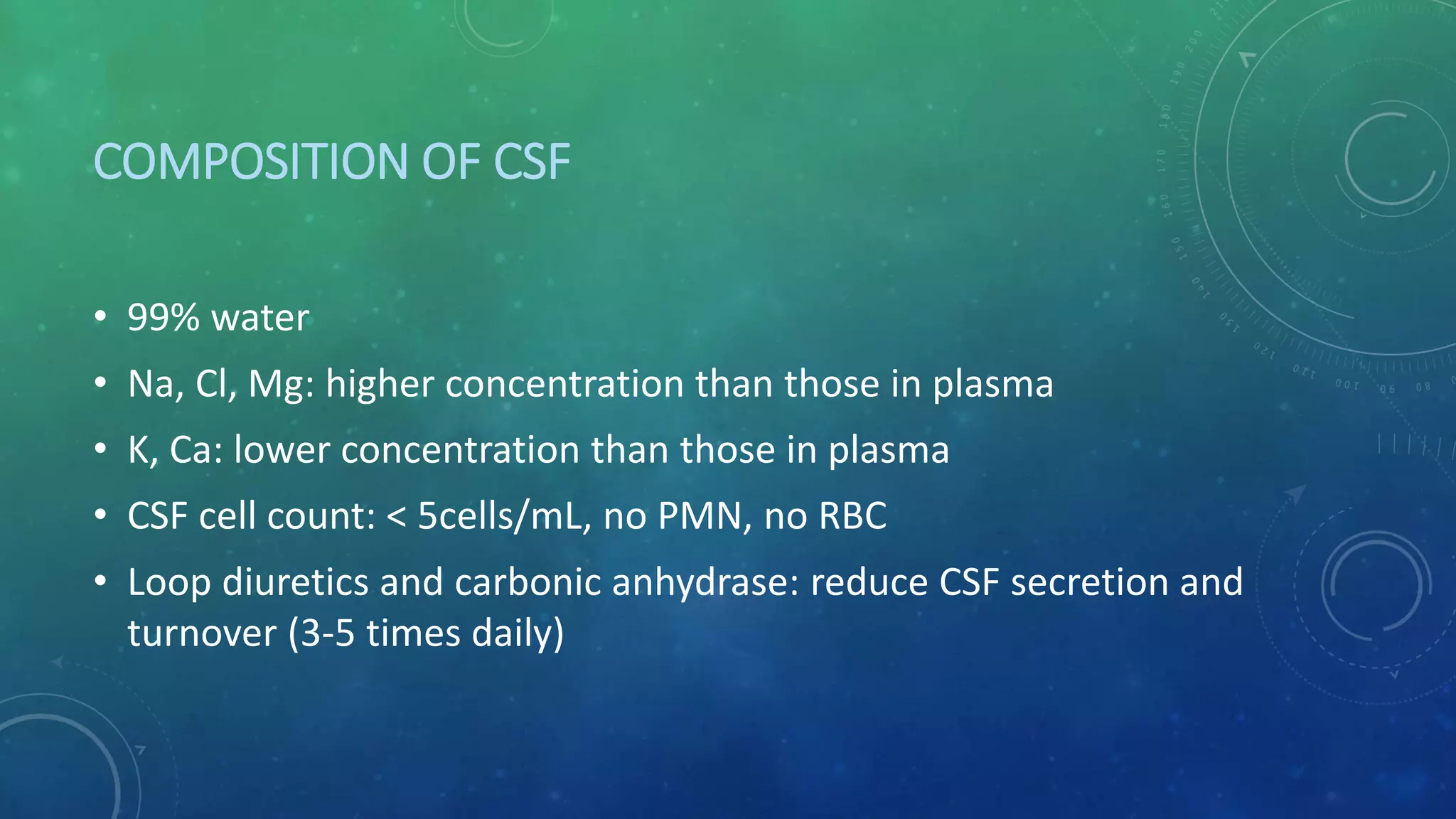
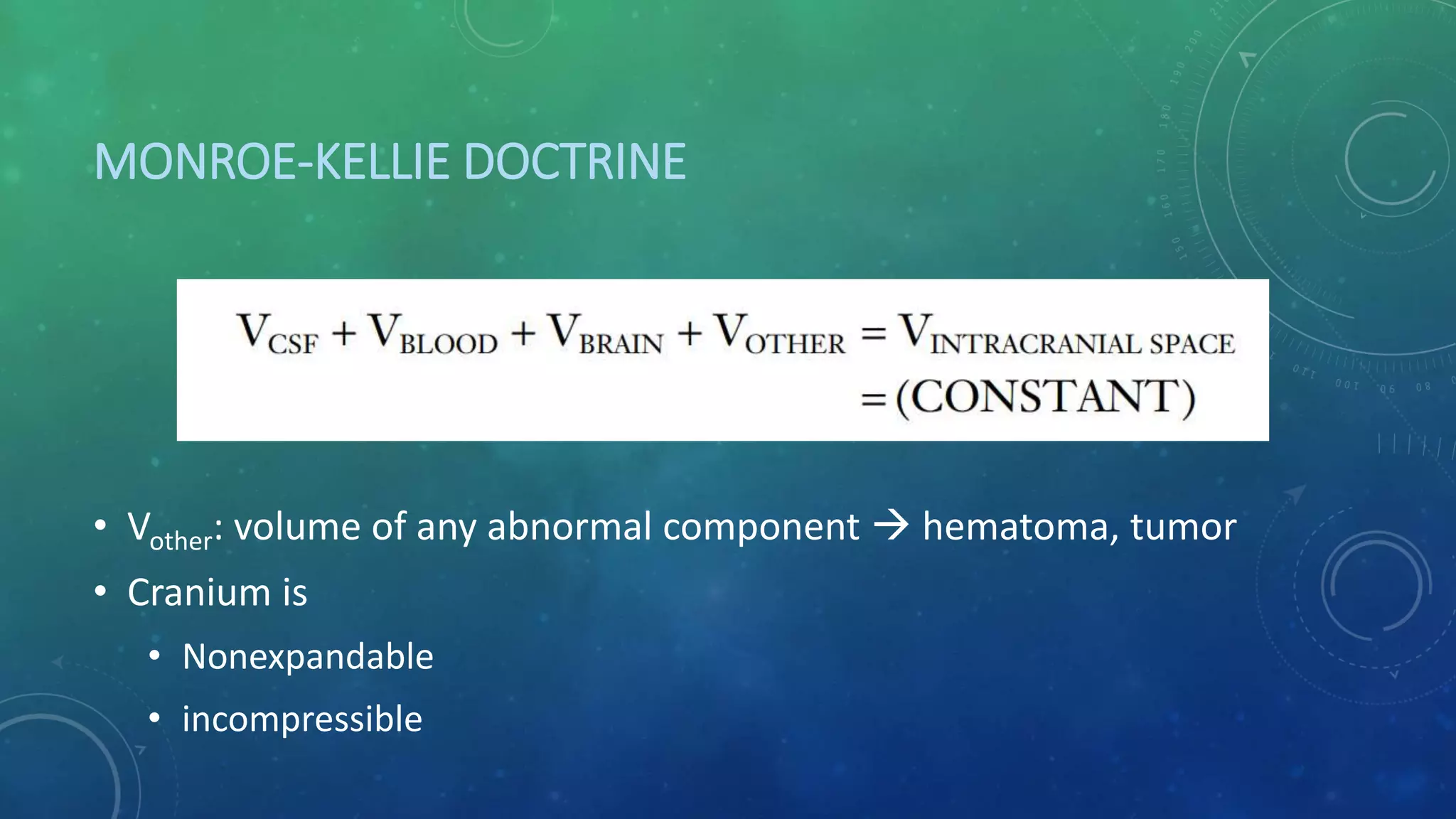
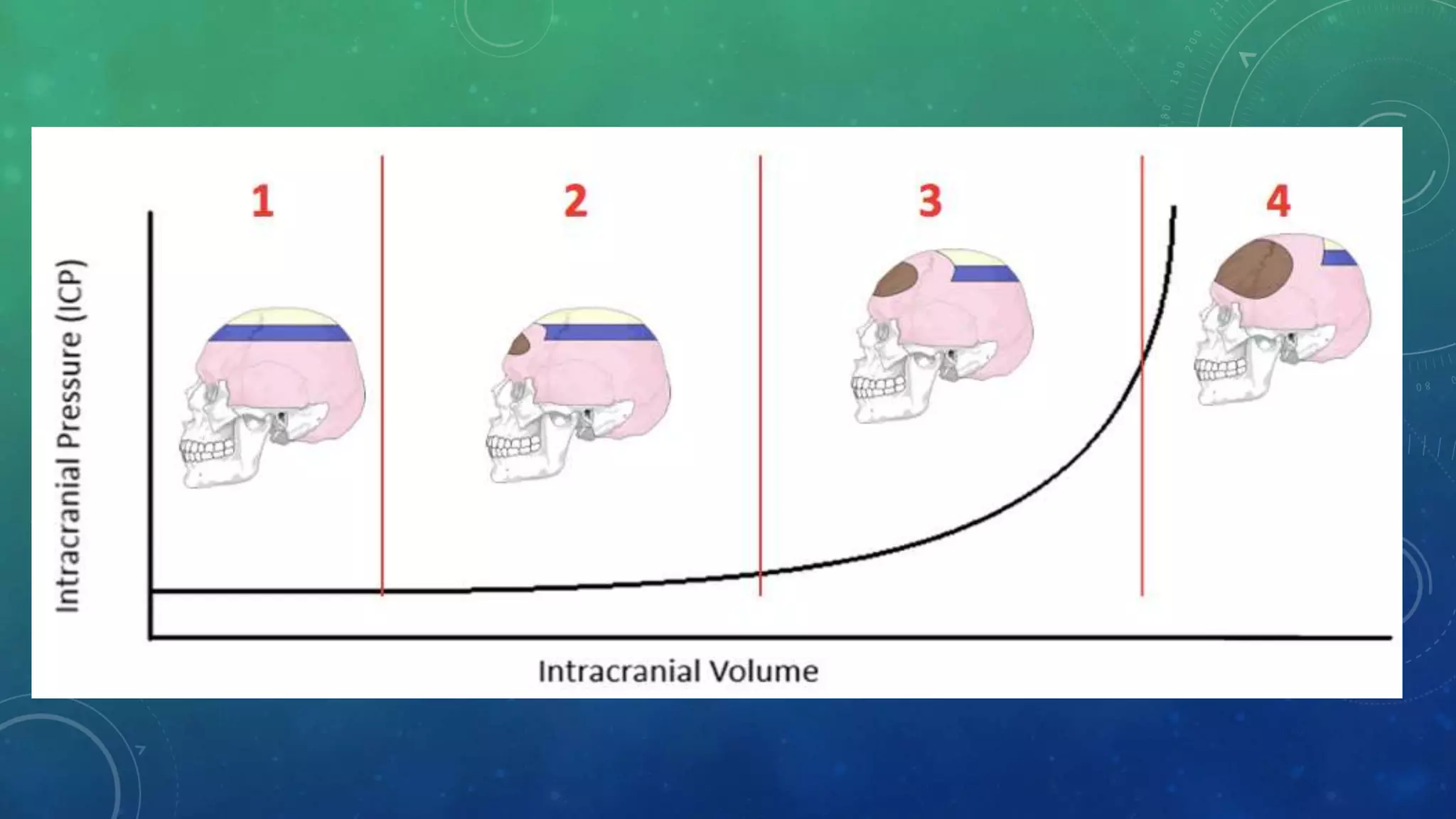
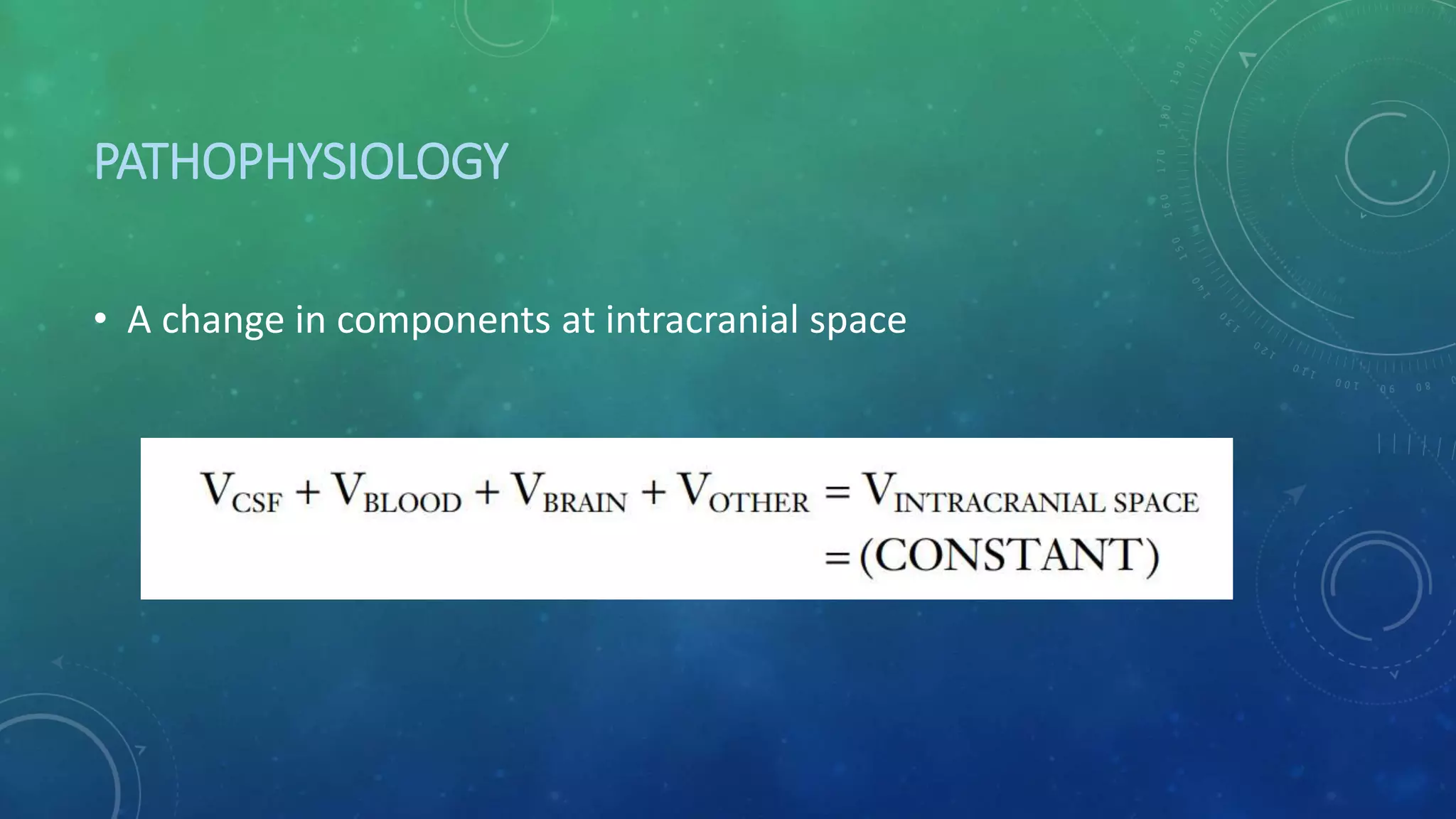
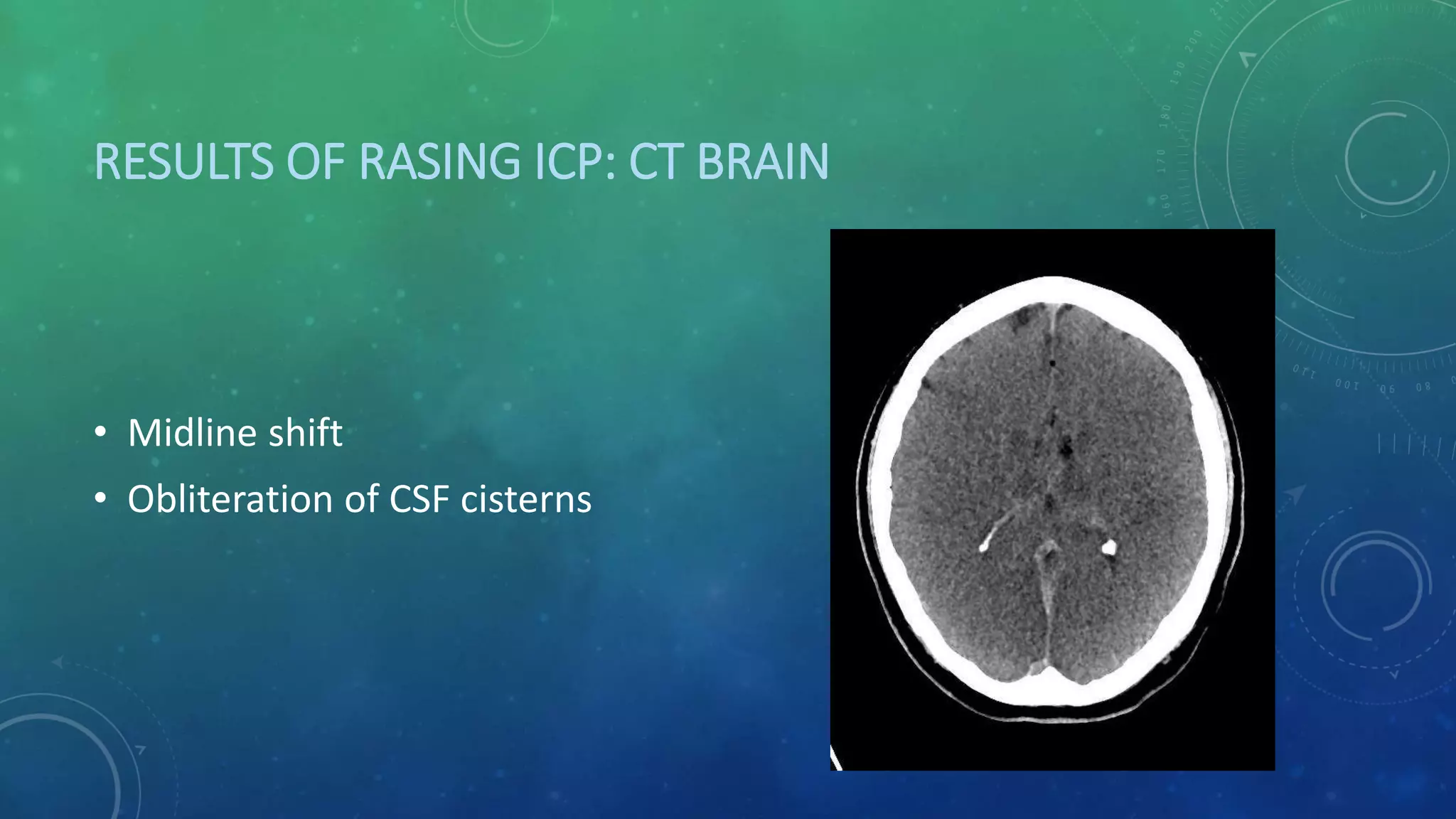
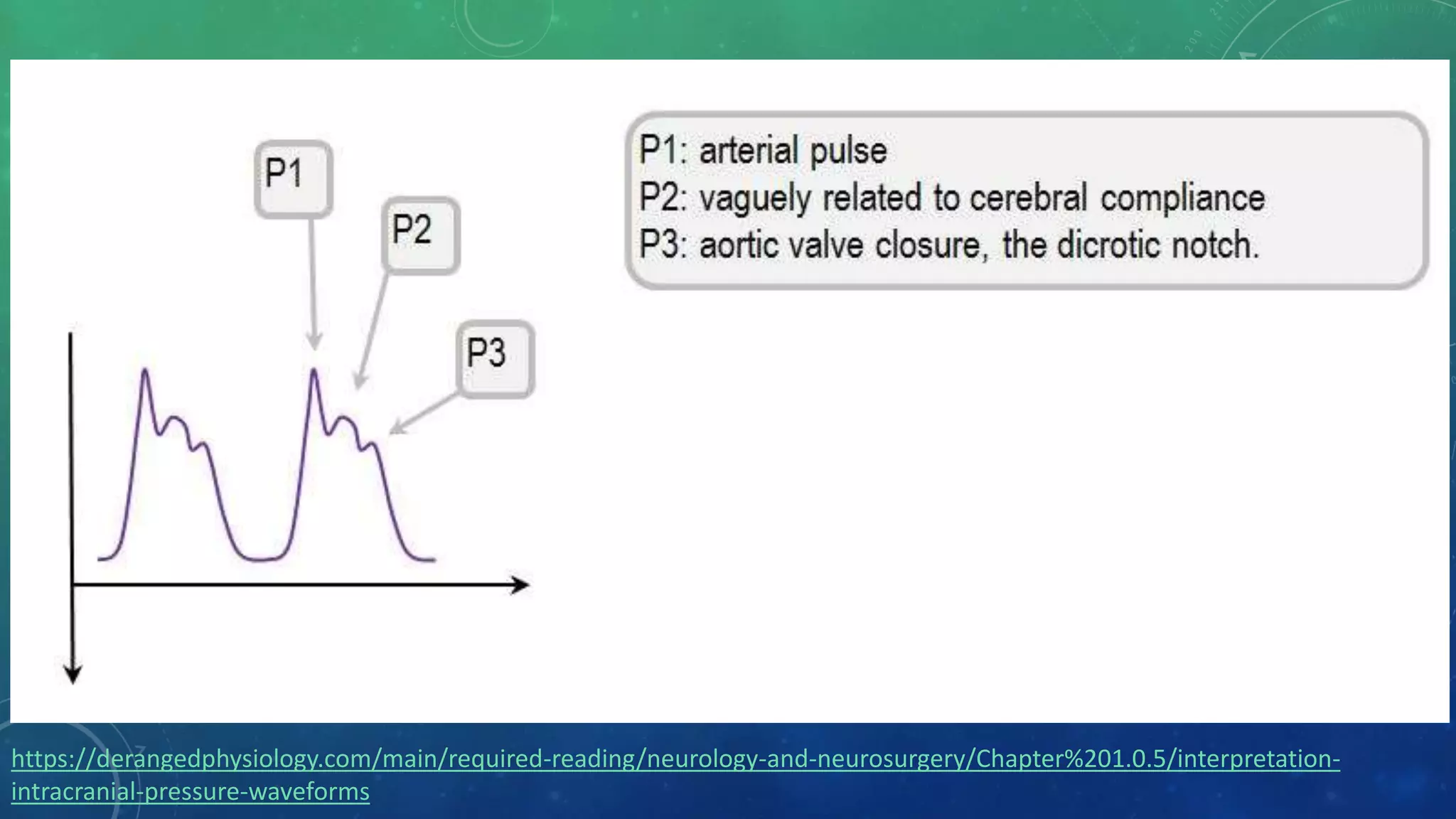
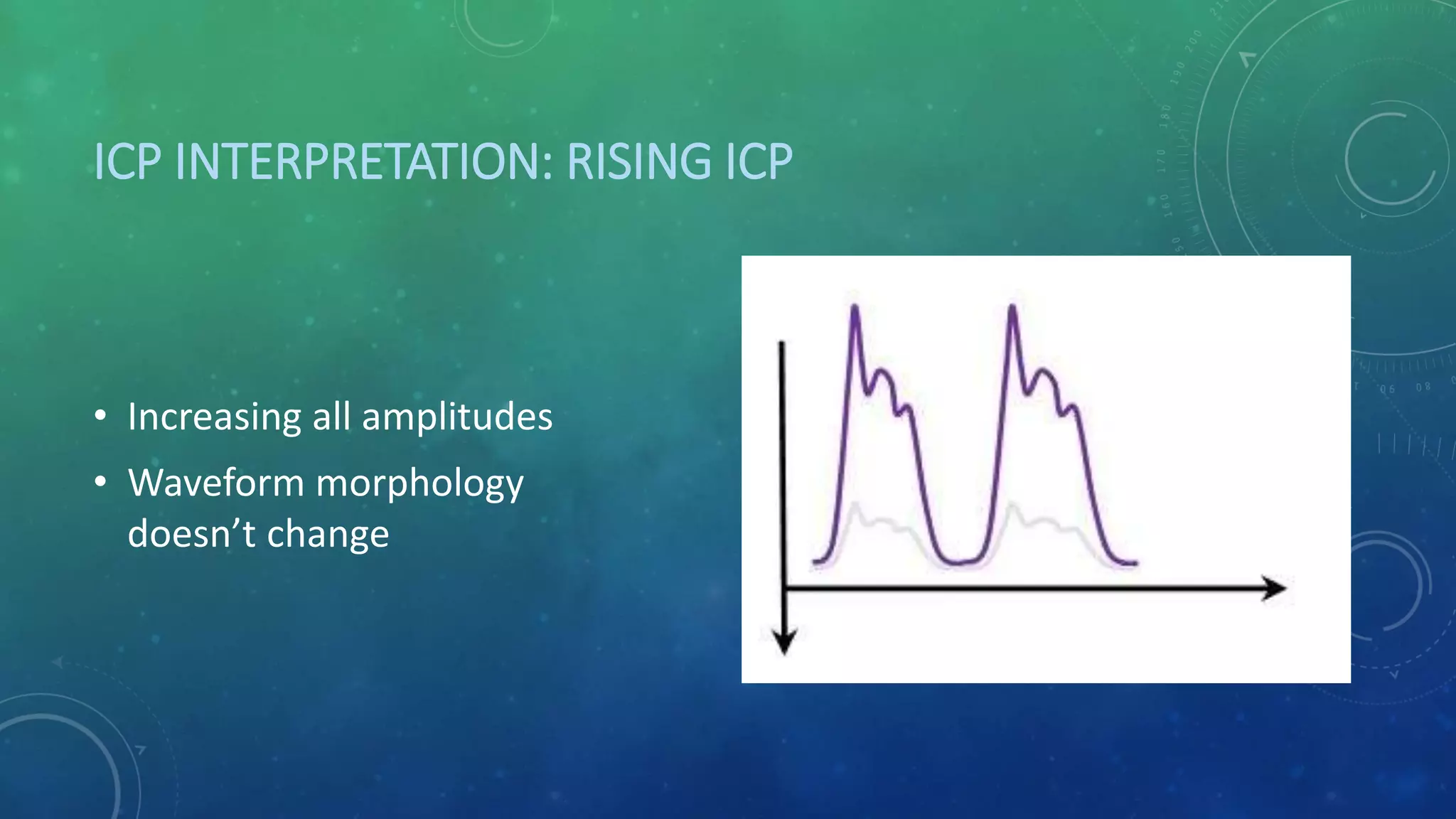
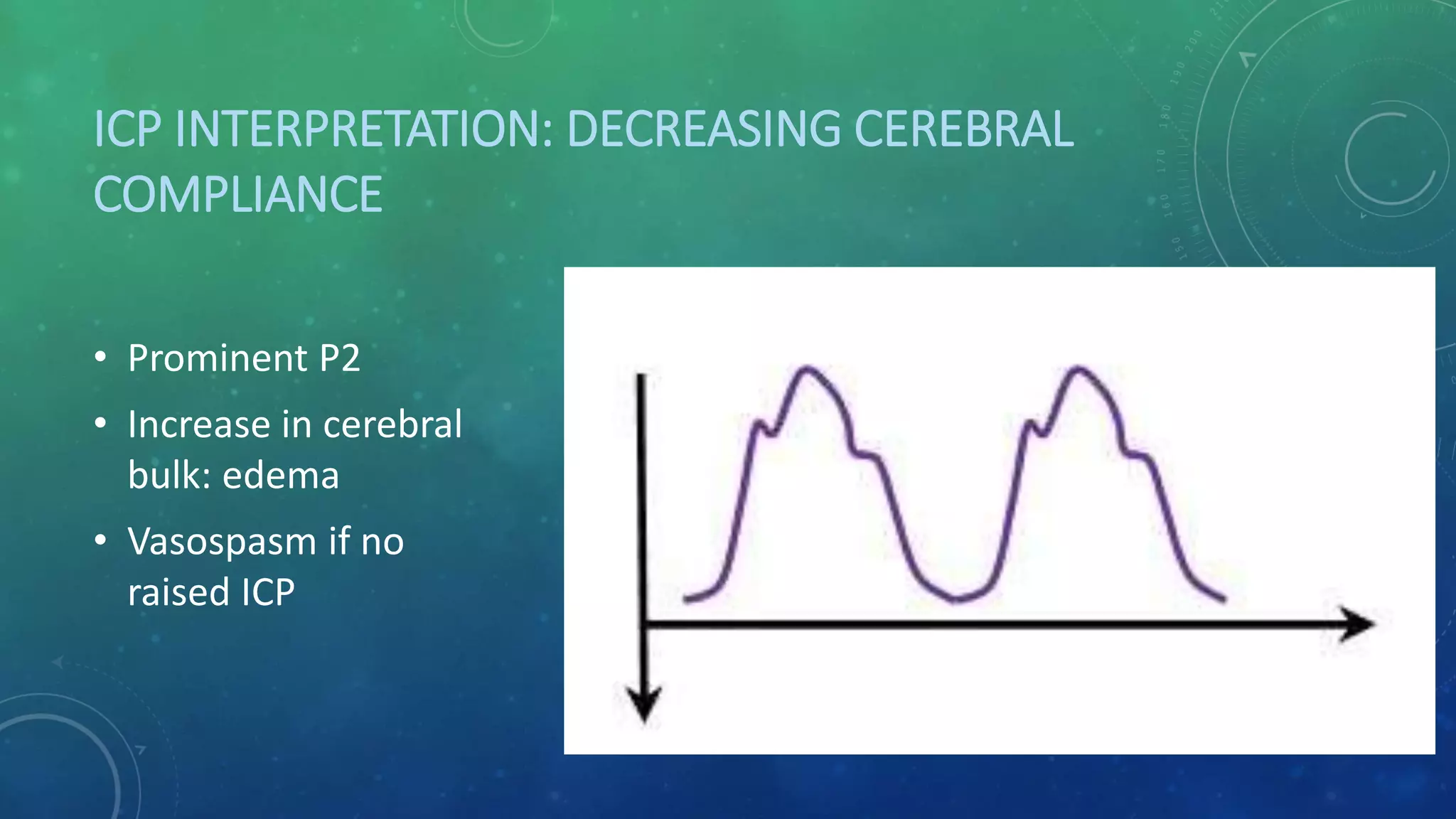
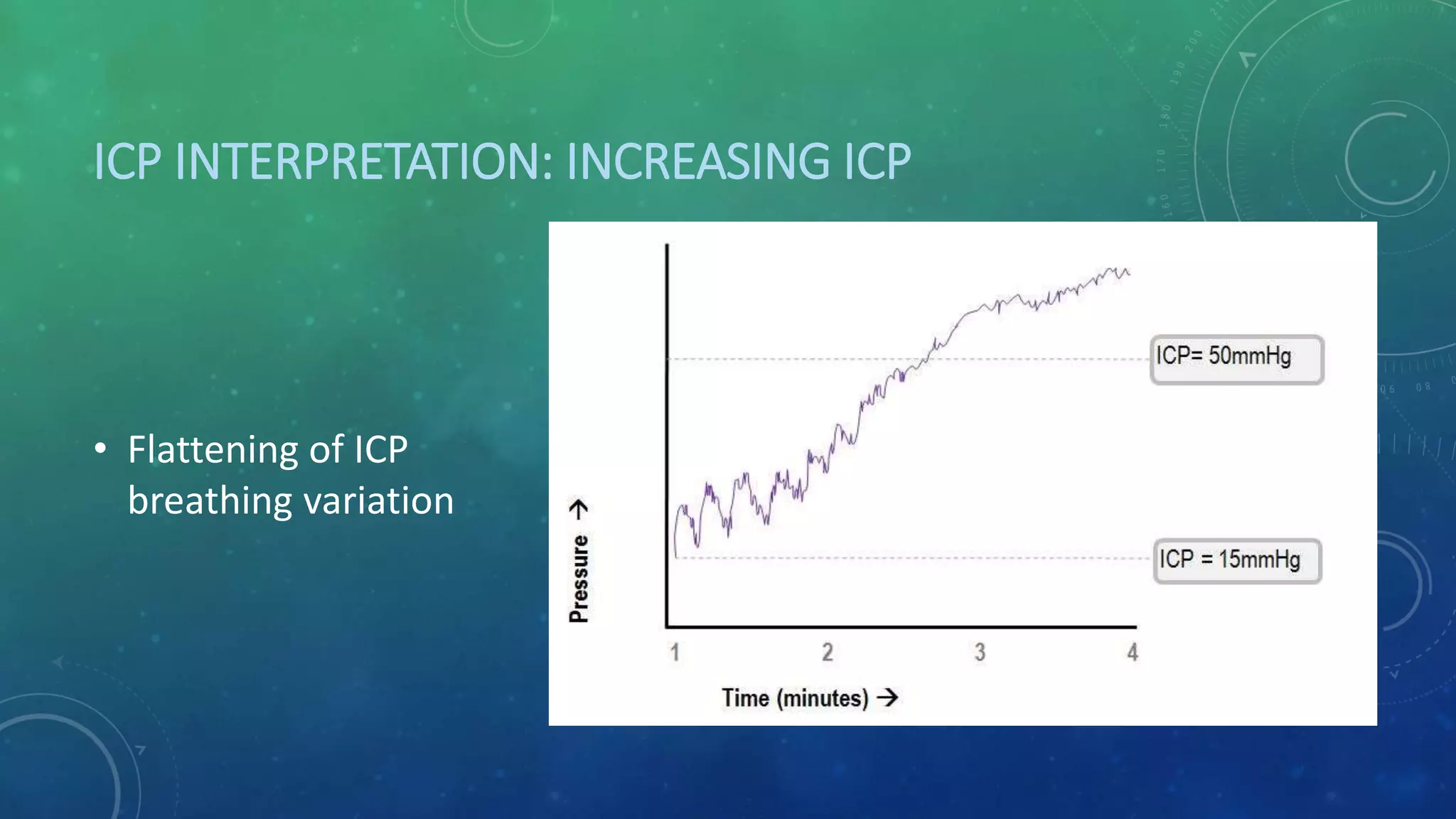
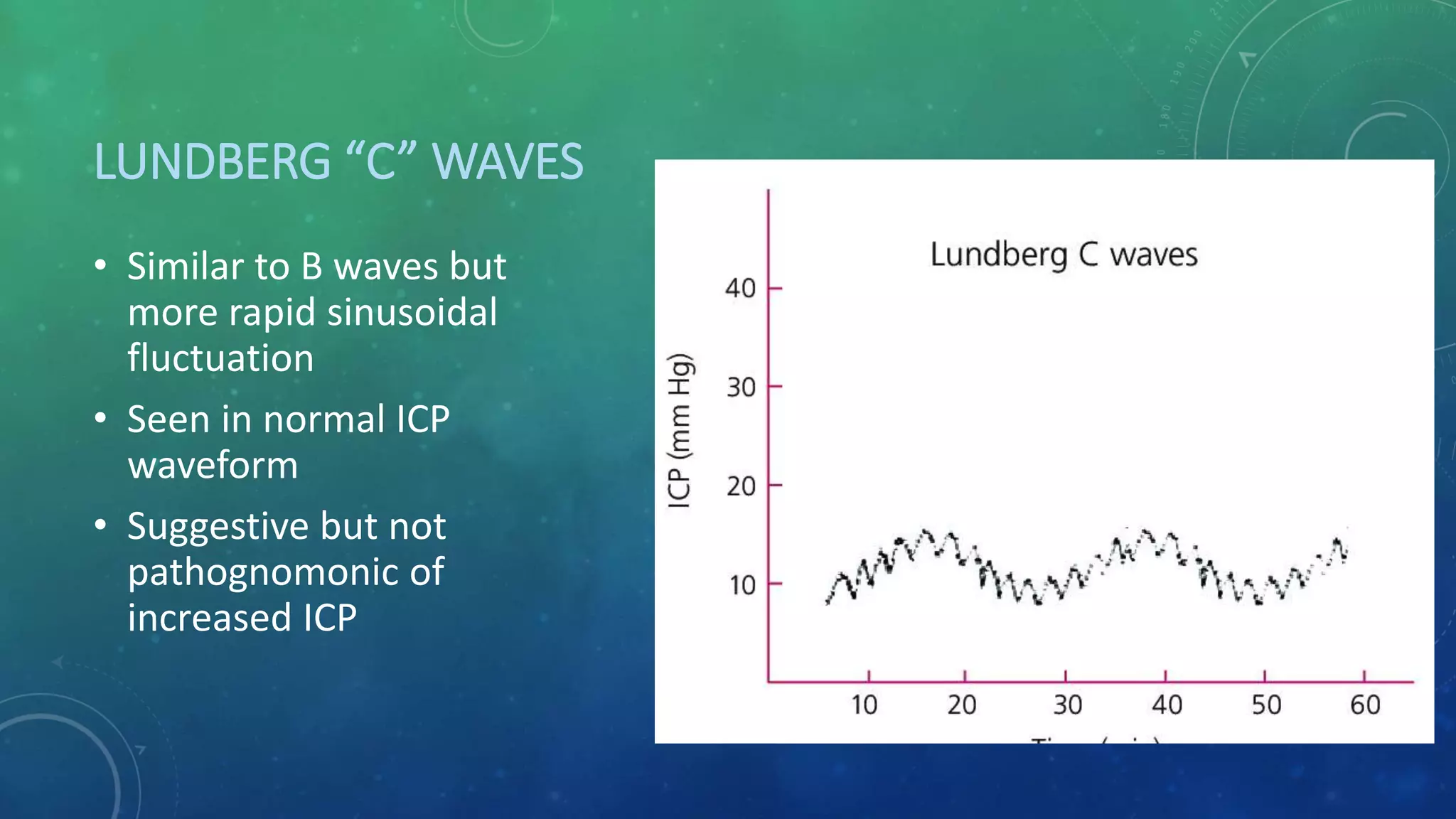
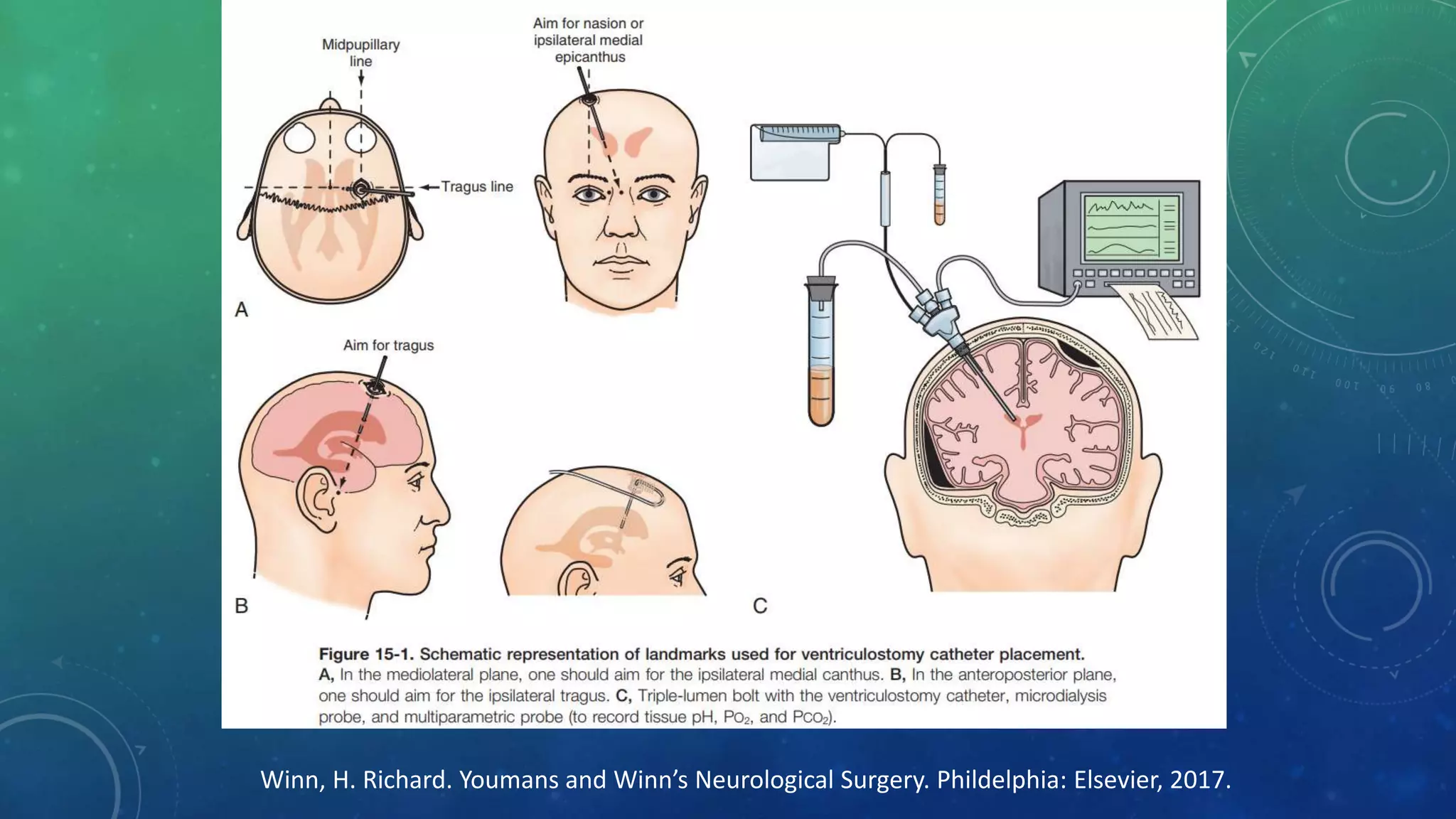
This document outlines the essentials of intracranial pressure (ICP), including the physiology of cerebrospinal fluid (CSF) production and flow, normal ICP physiology and the pathophysiology of increased ICP. It discusses ICP waveform interpretation, monitoring technologies and treatment of elevated ICP. CSF is produced by the choroid plexus and absorbed through arachnoid villi. ICP is regulated by the Monroe-Kellie doctrine. Increased ICP can result from mass lesions, edema, venous outflow obstruction or CSF abnormalities. ICP monitoring is most accurate via external ventricular drain. Treatment focuses on reducing CSF volume and space-occupying lesions while maintaining cerebral perfusion pressure.