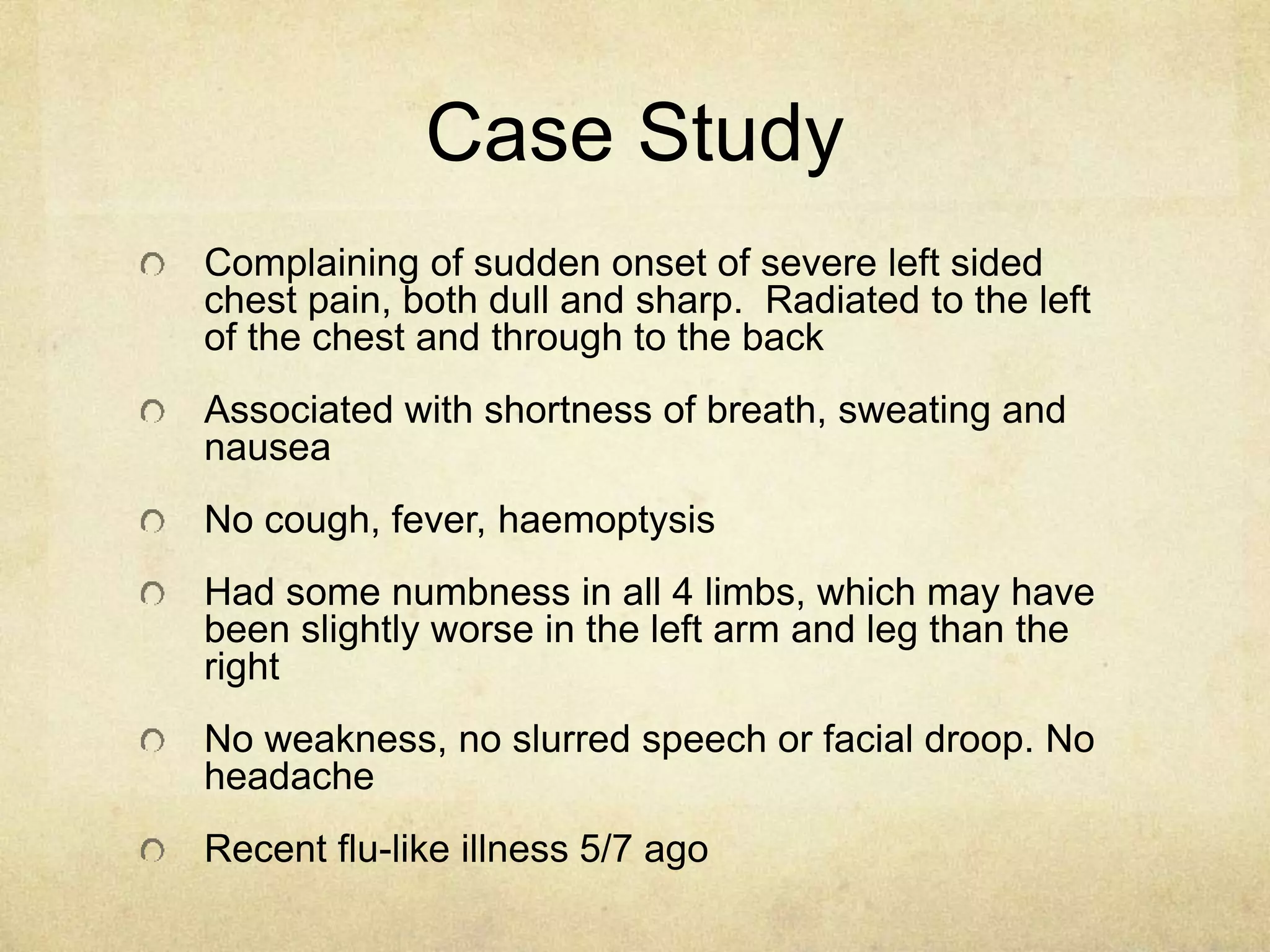
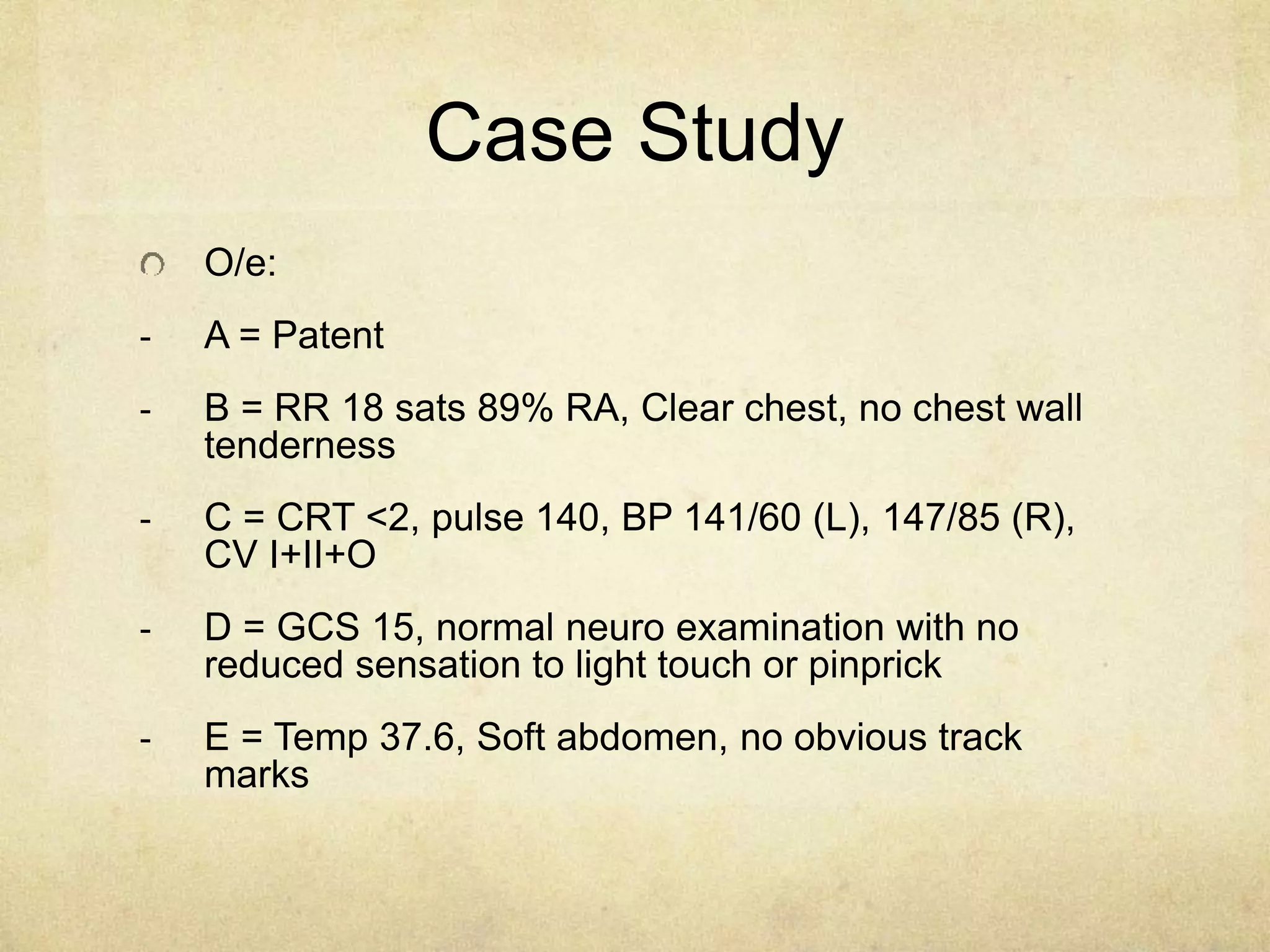
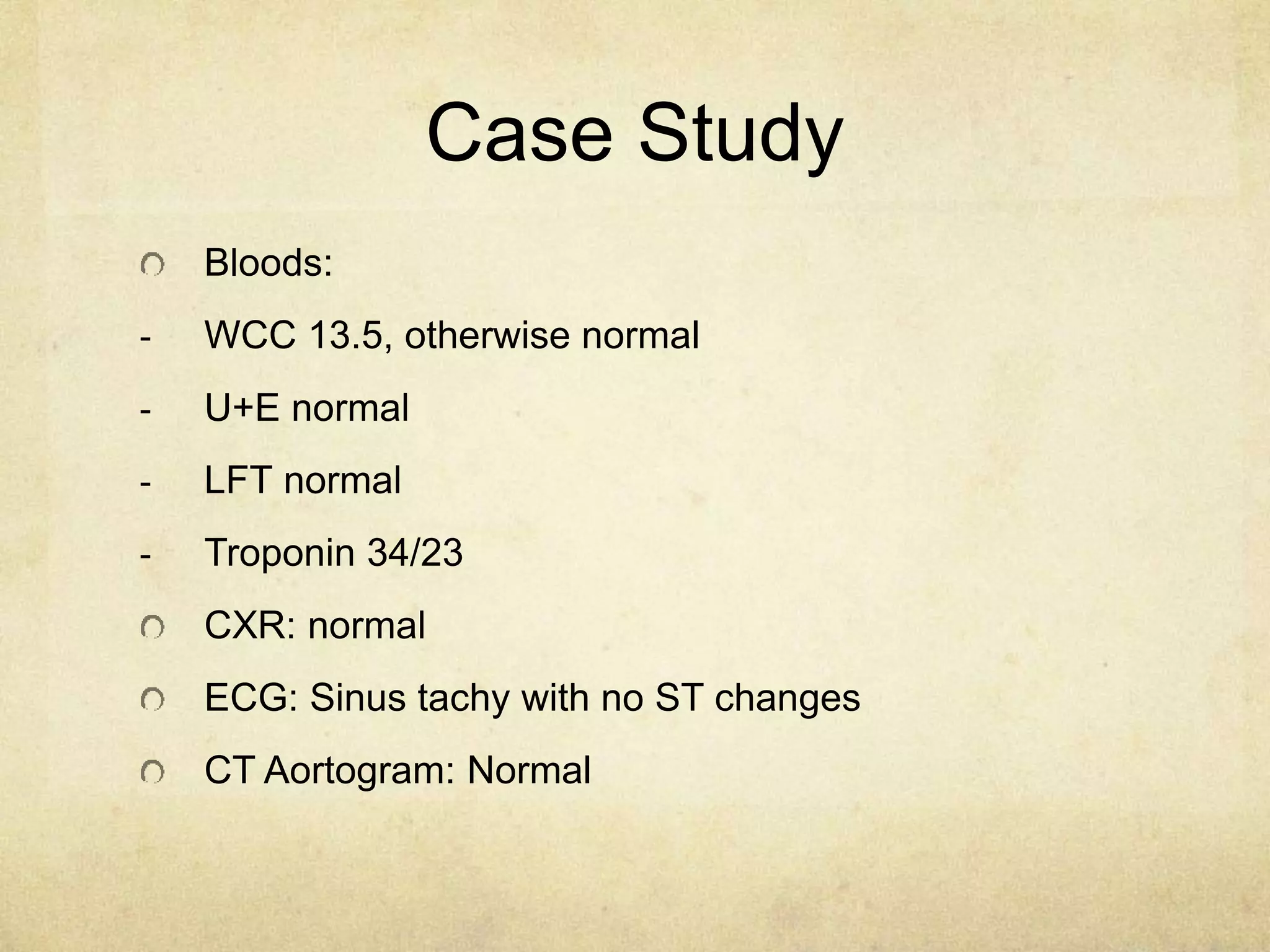
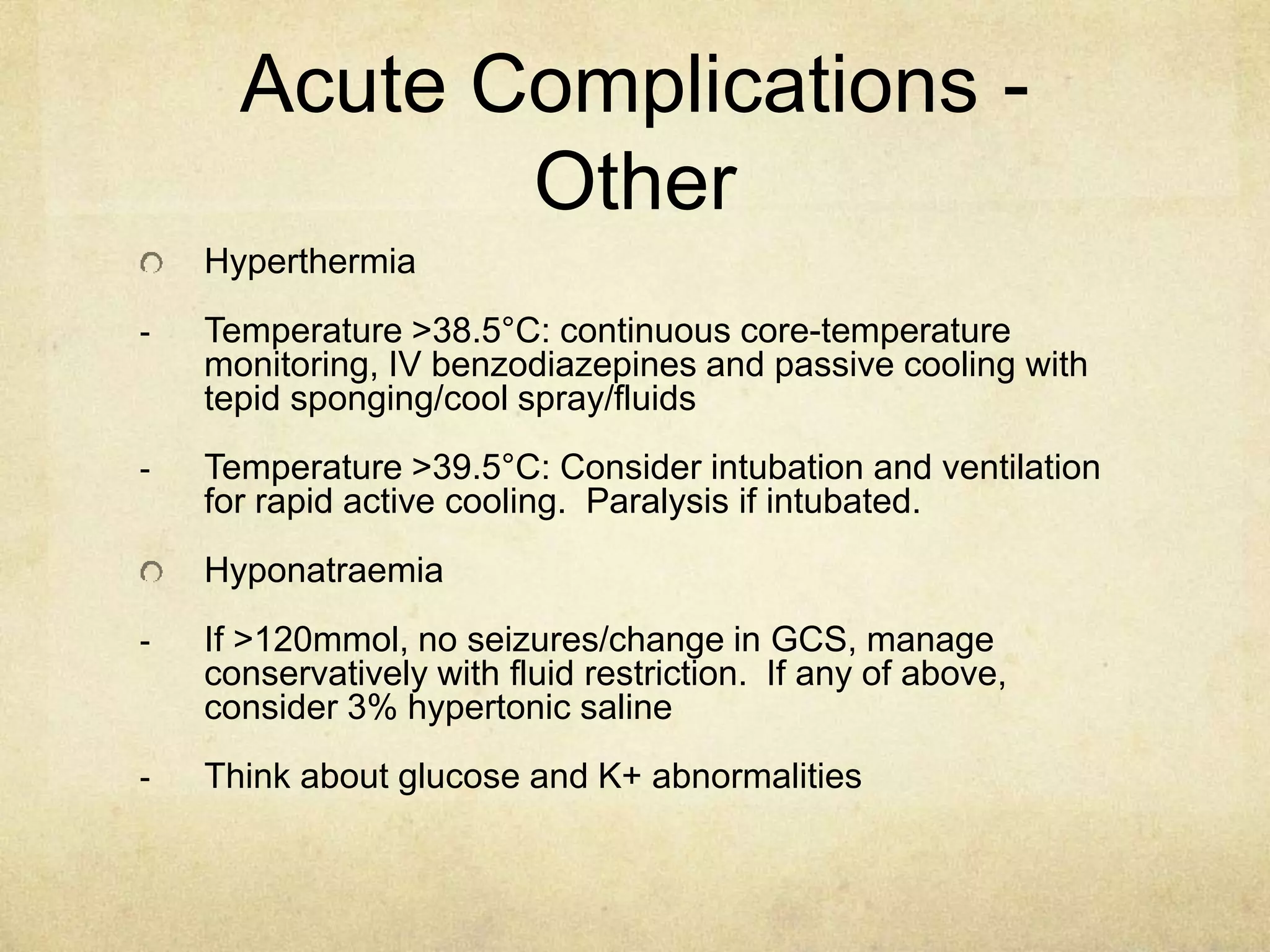
Amphetamine use is common in Australia, second only to cannabis. This presentation reviewed the history, epidemiology, and complications of amphetamine use and provided a case study. Acute complications include increased heart rate, blood pressure, arrhythmias, chest pain, agitation, psychosis, seizures, and hyperthermia. Chronic complications include increased risk of infections, stroke, heart disease, and mental health issues. Management involves monitoring vitals and giving benzodiazepines to treat agitation, seizures, and other complications.