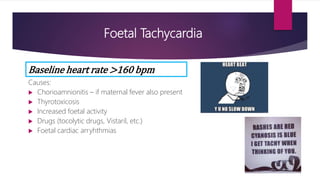
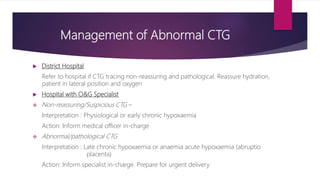
This document discusses various abnormal fetal heart rate patterns seen on a cardiotocography (CTG) tracing during labor and delivery. It describes fetal tachycardia as a heart rate over 160 bpm and potential causes like infection or drugs. Fetal bradycardia below 120 bpm is ominous and can be caused by hypoxia. Early decelerations occur with contractions and recover after, while late decelerations begin with contractions but recover slowly, indicating hypoxia. Variable decelerations can be caused by cord compression. Reduced variability may indicate fetal sleep, acidosis, or drugs. Management depends on whether the CTG is reassuring or pathological, with pathological cases requiring specialist evaluation and potential urgent delivery.