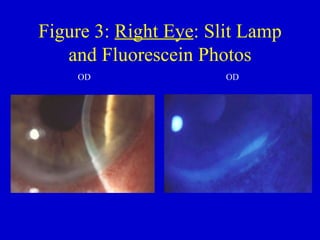
A 61-year-old man with a history of rheumatoid arthritis presented with redness, irritation, and blurred vision in his right eye. He was diagnosed with peripheral ulcerative keratopathy (PUK). His symptoms improved with oral steroids, topical steroids, ofloxacin drops, and bacitracin ointment. PUK is a rare inflammatory eye condition commonly associated with rheumatoid arthritis that involves breakdown of the cornea.