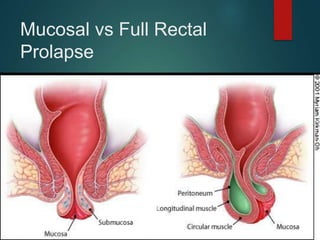
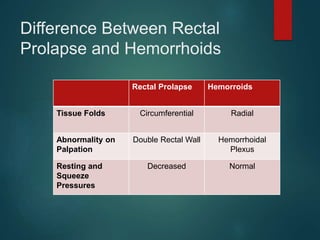
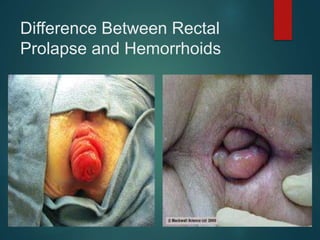
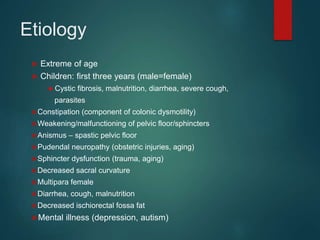
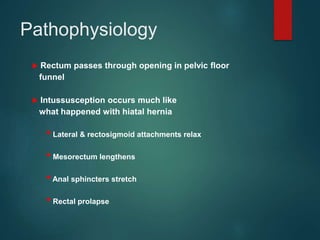
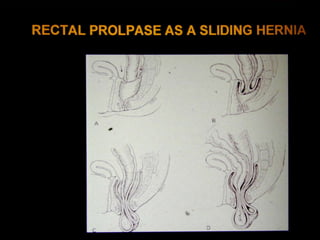
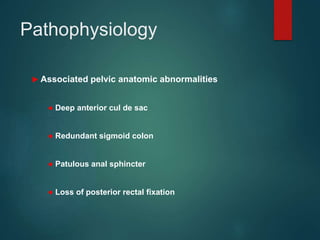
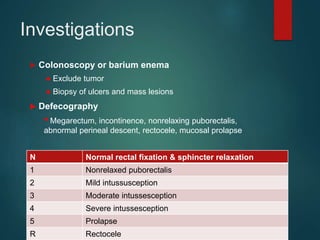
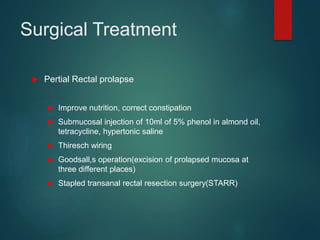
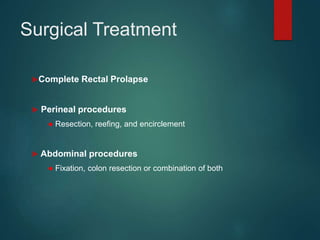
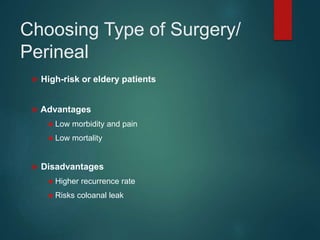
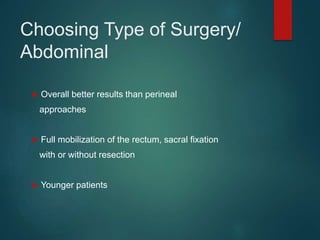
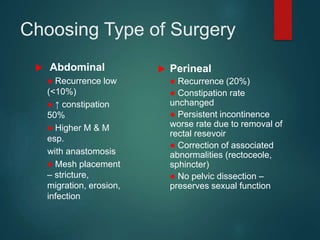
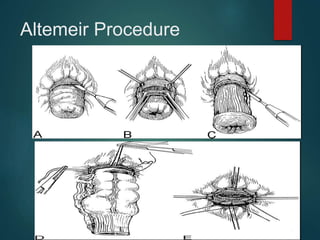
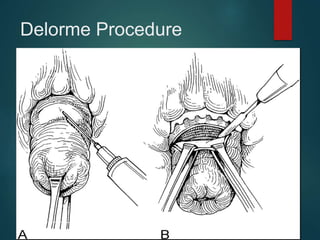
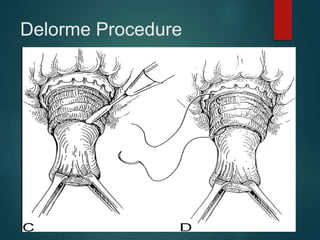
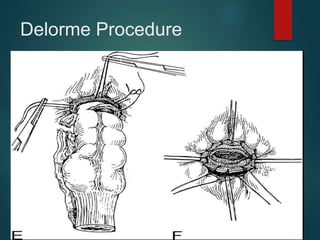
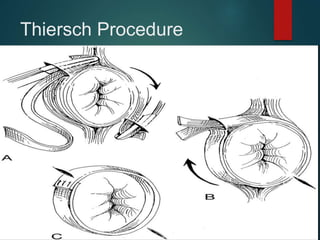
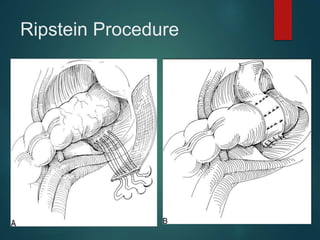
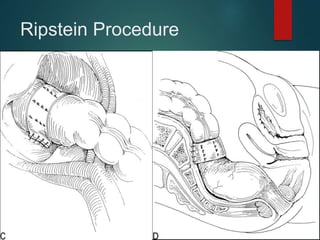
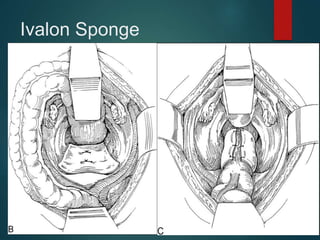
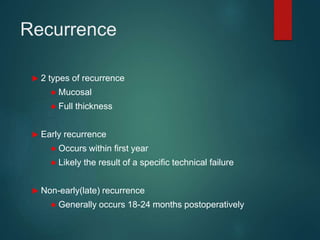
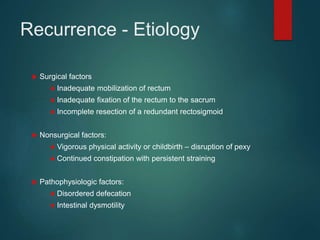
This document describes a case of rectal prolapse in a 15-year-old male patient who reported a mass coming out of his anus for the past 4 years. On examination, the doctor observed a pinkish mass coming out of the anus during straining that was soft and reducible. Rectal prolapse was included in the differential diagnosis along with large rectal polyp and hemorrhoids. The document proceeds to provide details on the types, causes, symptoms, evaluation, and management of rectal prolapse, including non-surgical and surgical treatment options such as perineal and abdominal procedures. Complications of treatment are also discussed.