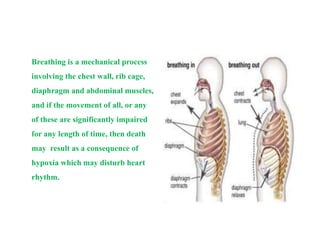
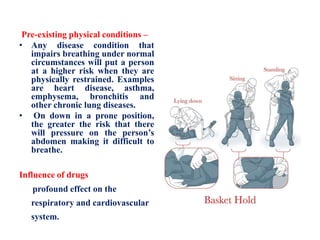
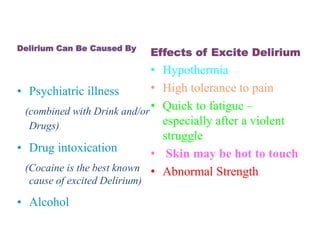
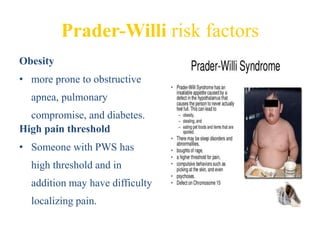
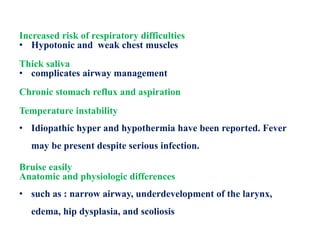
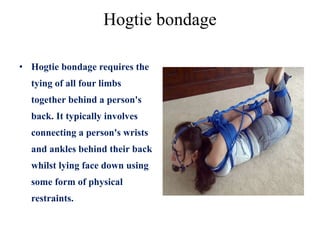
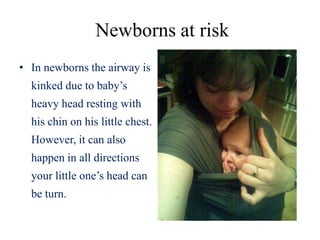
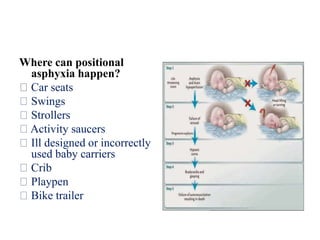
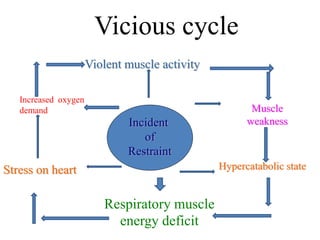
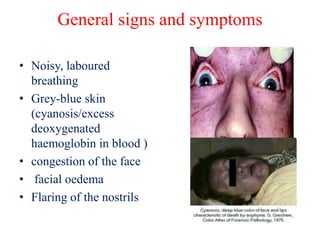
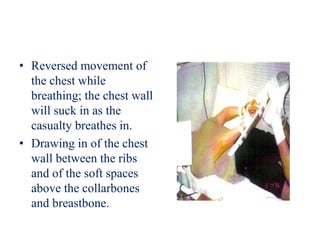
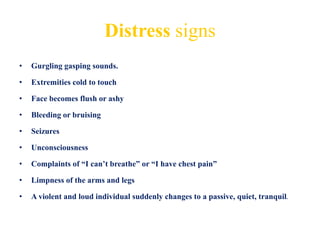
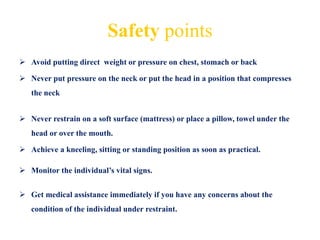
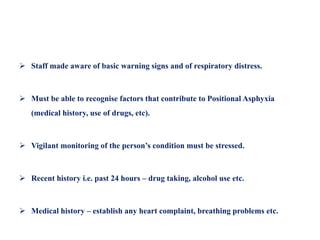
This document defines positional asphyxia as obstructing an restrained individual's airway or interfering with respiration, depriving them of oxygen. It can result from impaired movement of the chest wall, rib cage, diaphragm or abdominal muscles. Positional asphyxia has been associated with deaths during physical and mechanical restraint. Risk factors include prone positioning, prolonged struggle, intoxication, obesity, psychosis, pre-existing medical conditions, and drugs affecting respiration or cardiovascular systems. Signs may include labored breathing, cyanosis, weakness, and loss of consciousness. Safety requires avoiding chest/back pressure and head compression, monitoring vitals, and getting medical help for any respiratory distress concerns.