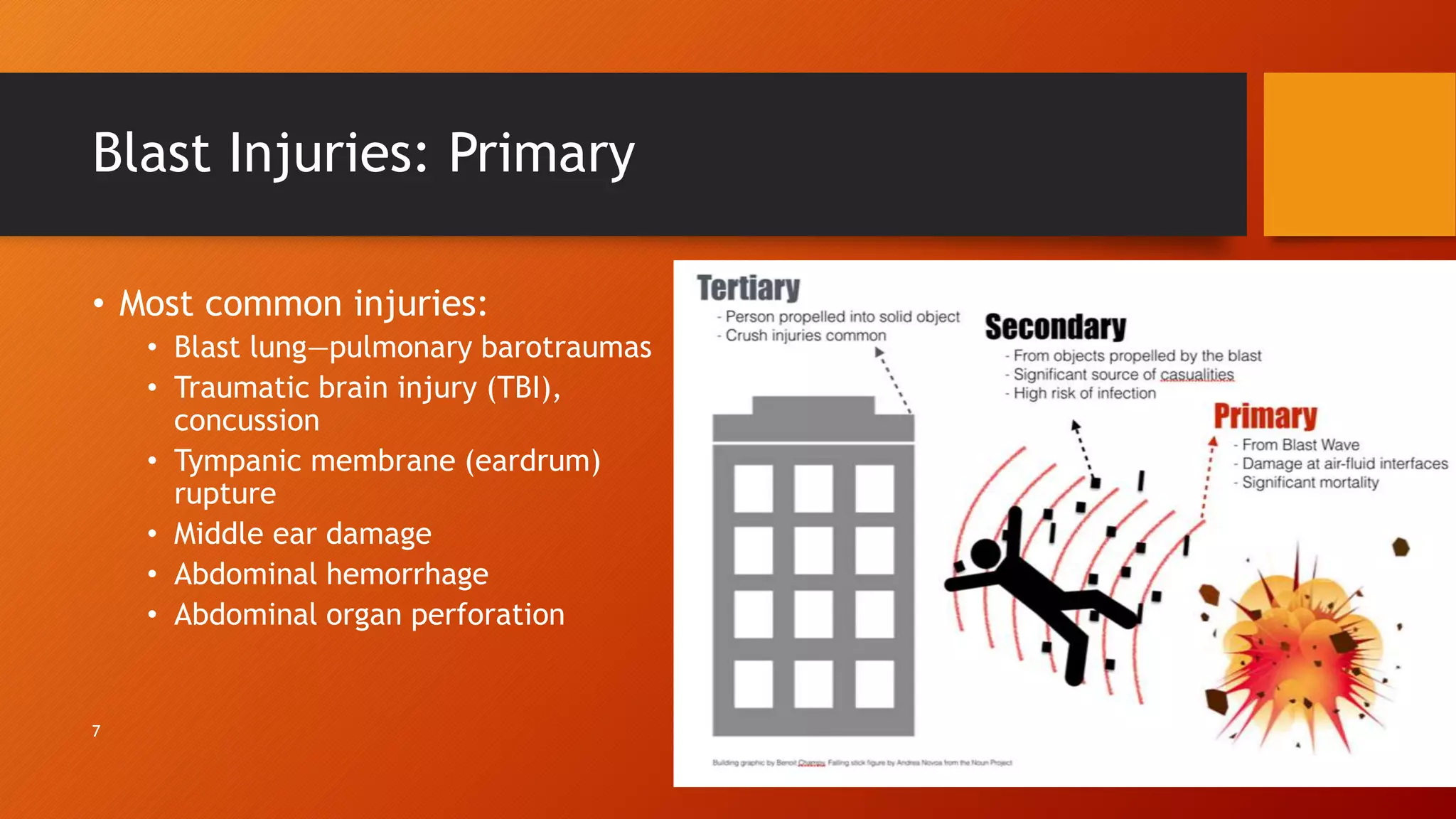
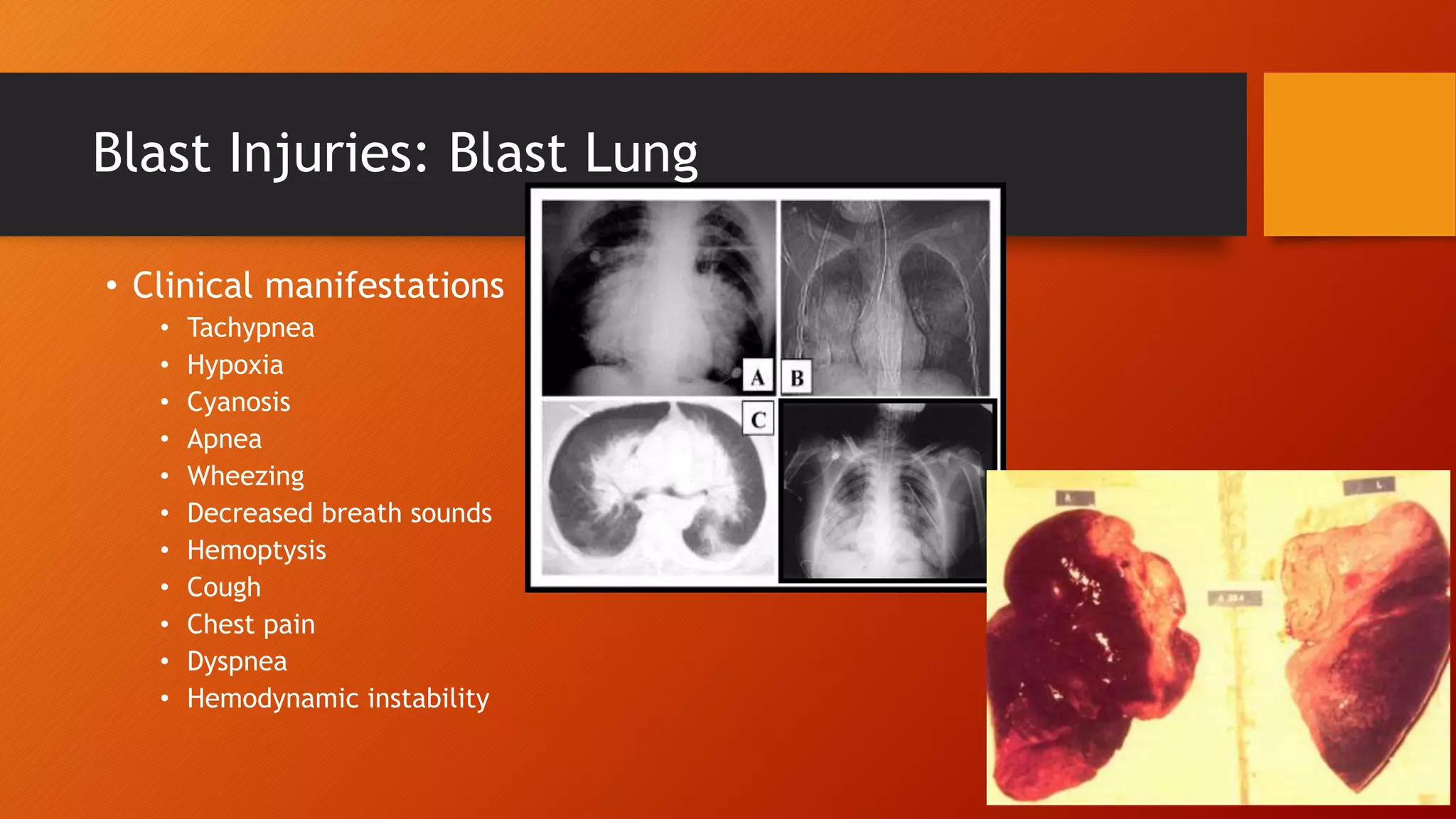
Blast injuries are caused by explosions and present unique challenges. They can be categorized as primary, secondary, tertiary or quaternary injuries depending on the mechanism. Primary injuries are caused directly by the blast wave and can include blast lung and traumatic brain injury. Secondary injuries are caused by flying debris and result in penetrating wounds. Tertiary injuries occur when individuals are thrown by the blast wind, causing fractures or amputations. Quaternary injuries include burns, exacerbation of medical conditions, and complications. Management requires assessing the type of explosive, victim location, signs of inhalation injury, and initiating triage, treatment and evacuation.