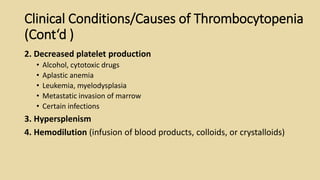
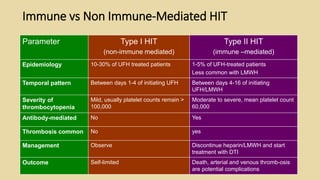
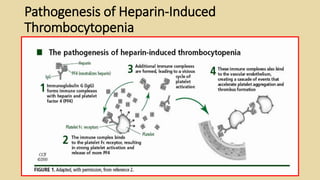
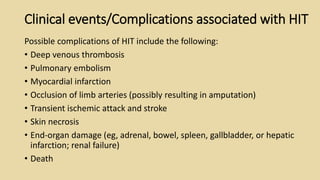
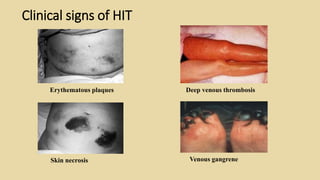
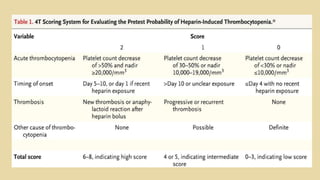
This document provides information about heparin-induced thrombocytopenia (HIT). It begins by introducing HIT as an immune-mediated reduction in platelet count that occurs in 3-5% of patients receiving unfractionated heparin for 5 days or more, and less than 1% for low molecular weight heparin. It then describes HIT as characterized by a platelet decrease of over 50% from baseline 5-10 days after starting heparin, along with hypercoagulability and heparin-dependent antibodies. The document outlines the pathogenesis of HIT and differences between type I and type II, reviews potential clinical complications, diagnostic methods, and emphasizes the need to promptly discontinue heparin and